Abstract
Background
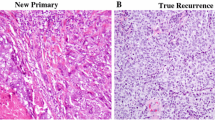
Ipsilateral breast tumor recurrences (IBTR) after breast-conserving treatment include two different entities: true recurrence (TR) thought to occur when residual cancer cells grow gradually to detectable size and new primary (NP) thought to be de novo cancer independently arising in the preserved breast. The patients with ipsilateral breast tumor recurrence (IBTR) are potentially at high risk for subsequent distant metastasis, but many studies do not distinguish between these types of recurrence. The aim of this study is to clarify the biological difference between TR and NP, and to show the clinical significance of classifying IBTR into these two types of recurrence.
Patients and Method
A total of 172 patients with IBTR after breast-conserving therapy from the cohort of a long-term large scale study (Research of cancer treatment from the Ministry of Health, Labor and Welfare of Japan (no.13–9)) were analyzed. We classified IBTRs as TR or NP based on tumor location and pathological findings. The characteristics of the primary tumors of TR and NP were compared. Survival rates and risk factors of each type of IBTR were examined by the Kaplan-Meier method. The results of salvage surgery were also analyzed.
Results
Of the 172 patients, 135 patients were classified as TR and 26 as NP. Eleven cases could not be categorized. The primary tumor of TR was characterized by a high rate of lymph node metastasis (37.8%) and short disease-free interval (mean DFI; 46.6 months) while that of NP showed a rather low lymph node positivity (8.7%) and longer DFI (62.1 months). The risk factors for TR were young age, positive surgical margin, omission of irradiation and positive lymph node metastasis. Those for NP were young age, omission of irradiation and contralateral breast cancer after the primary operation. The 5-year survival rates after IBTR were 71.0% in TR and 94.7% in NP (p=0.022). Salvage operation was performed in 136 IBTRs. Eighty-one patients underwent salvage mastectomy and 55 patients underwent repeat lumpectomy. Five-year survival rates after salvage operation were 75.7% for mastectomy and 84.2% for lumpectomy (N.S.). Twenty percent of patients who underwent repeat lumpectomy developed secondary local relapse within 5 years after salvage treatment The risk factors for secondary local relapse were analyzed. Limited to cases of IBTR which received radiation therapy after the primary operation, NP was the only factor influencing secondary local relapse by univariate analysis.
Conclusions
TR and NP show clinically quite different features; time to occurrence, characteristics of the original tumor, prognosis and risk factor profile for IBTR were all different. Classifying IBTR as TR or NP can provide clinically significant data for the management of IBTR.
Similar content being viewed by others
References
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER,et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectpmy, and lumpectomy plus irradiation for the treatment of invasive breast cancer.N Engl J Med 347:1233–1241, 2002.
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A,et al: Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer.N Engl J Med 347:1227–1232, 2002.
Fowble B: Ipsilateral breast tumor recurrence following breast-conserving surgery for early-stage invasive cancer.Acta Oncol 38 Suppl 13:9–17, 1999.
Mamounas E: Ipsilateral breast tumor recurrence after lumpectomy: Is it time to take the bull by the horns?J Clin Oncol 19:3798–3800, 2001.
Lannin DR, Haffty BG: End results of salvage therapy after failure of breast-conservation surgery.Oncology 18:272–279, 2004.
Kurtz JM, Spitalier JM, Amalric R, Brandone H, Ayme Y, Jacquemier J,et al: The prognostic significance of late local recurrence after breast-conserving therapy.Int J Radiat Oncol Biol Phys 18:87–93, 1990.
Freedman GM, Fawble B: Local recurrence after mastectomy or breast-conserving surgery and radiation.Oncology 14:1561–1581, 2000.
Touboul E, Buffat L, Belkacemi Y, Lefranc JP, Uzan S, Lhuillier P,et al: Local recurrences and distant metastases after breast-conserving surgery and radiation therapy for early breast cancer.Int J Radiat Oncol Biol Phys 46:683–684, 2000.
Fisher B, Anderson S, Fisher ER, Redmond C, Wickerham DL, Wolmark N,et al: Significance of ipsilateral breast tumor recurrence after lumpectomy.Lancet 338:327–331, 1995.
Veronesi U, Marubini E, VecchioDel M, Manzari A, Andreola S, Greco M, Luini A,et al: Local recurrences and distant metastases after conservative breast cancer treatments: partly independent events.J Natl Cancer Inst 87: 19–27, 1995.
Schmoor C, Sauerbrei W, Bastert G, Schmoor M: Role of isolated locoregional recirrence of breast cancer: Results of four prostictive studies.J Clin Oncol 18:1696–1708, 2000.
Bethke KP: Breast Conservation: predictors and treatment of local recurrence.Semin Surg Oncol 12:332–338, 1996.
Kurtz JM, Jacquemier J, Amalric R, Brandone H, Ayme Y, Hans D,et al: Is breast conservation after local recurrence feasible?Eur J Cancer 27:240–244, 1991.
Salvadori B, Marubini E, Miceri R, Cont AR, Cusumano F, Andreola S,et al: Reoperation for locally recurrent breast cancer in patients previously treated with conservsative surgery.Br J Surg 86:84–87, 1999.
Clemons M, Hamilton T, Mansi J, Lockwood G, Goss P: Management of recurrent locoregional breast cancer: oncologist survey.Breast 12:328–337, 2003.
Delia Rovere GQ, Benson RJ: Ipsilateral breast tumor recurrence of breast cancer: determinant or indicator of poor prognosis.Lancet Oncol 3:183–187, 2002.
Smith TE, Lee D, Turner BC, Carter D, Haffty BG: True recurrence vs. new primary ipsilateral breast tumor relapse: an analysis of clinical and pathologic differences and their implications in natural history, prognoses, and therapeutic management.Int J Radiat Oncol Biol Phys 48:1281–1289, 2000.
Santiago RJ, Wu L, Harris E, Fox K, Schultz D, Glick J,et al: Fifteen-year results of breast-conserving surgery and definitive irradiation for Stage I and II breast carcinoma: the University of Pennsylvania experience.Int J Radiat Oncol Biol Phys 58:233–240, 2004.
Recht A, Silen W, Schnitt SJ, Connolly JL, Gelman RS, Rose MA,et al: Time-course of local recurrence following conservative surgery and radiotherapy for early stage breast cancer.Int J Radiat Oncol Biol Phys 15:255–261, 1988.
Huang E, Buchholz TA, Meric F, Krishnamurthy S, Mirza NQ, Ames FC,et al: Classifying local disease recurrences after breast conservation therapy based on location and histology: new primary tumors have more favorable outcomes than true local disease recurrences.Cancer 95:2059–2067, 2002.
Chaudary MA, Millis RR, Hoskins EO, Haldor M, Bulbrook RD, Cuzick J: Bilateral primary breast cancer: A prospective study of disease incidence.Br J Surg 71:711–714, 1984.
Schlechter BI, Yang Q, Larson PS, Golubeva A, Blanchard RA, Morenas de La AI,et al: Quantitative DNA fingerprinting may distinguish new primary breast cancer from disease recurrence.J Clin Oncol 22:1830–1838, 2004.
Haffty BG, Carter D, Flynn SD, Fischer DB, Brash DE, Simons J,et al: Local recurrence versus new primary: Clinical analysis of 82 breast relapses and potential applications for genetic fingerprinting.Int J Radiot Oncol Biol Phys 27:575–583, 1993.
Fowble B, Solin L, Schultz D, Rubenstein J, Goodman RL: Breast recurrence following conservative surgery and radiation. Patterns of failure, prognosis, and pathologic findings from mastectomy specimens with implications for treatment.Int J Radiat Oncol Biol Phys 19:833–842, 1990.
Krauss DJ, Kestin LL, Mitchell C, Martinez AA, Vicini FA: Changes in temporal patterns of local failure after breast-conserving therapy and their prognostic implications.Int J Radiat Oncol Biol Phys 60:731–740, 2004.
Komoike Y, Motomura K, Inaji H, Kasugai T, Koyama H: Repeat lumpectomy for patients with ipsilateral breast tumor recurrence after breast-conserving surgery. Preliminary results.Oncology 64:1–6, 2003.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Komoike, Y., Akiyama, F., lino, Y. et al. Analysis of ipsilateral breast tumor recurrences after breast-conserving treatment based on the classification of true recurrences and new primary tumors. Breast Cancer 12, 104–111 (2005). https://doi.org/10.2325/jbcs.12.104
Issue Date:
DOI: https://doi.org/10.2325/jbcs.12.104