Abstract
Purpose
To identify prognostic factors after hepatocellular carcinoma (HCC) recurrence after liver transplantation (LT).
Methods
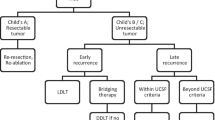
We retrospectively reviewed the combined experience at Toronto General Hospital and Hospital Vall d’Hebron managing HCC recurrence after LT (n = 121) between 2000 and 2012. We analyzed prognostic factors by uni- and multi-variate analysis. Median follow-up from LT was 29.5 (range 2–129.4) months. Median follow-up from HCC recurrence was 12.2 (range 0.1–112.5) months.
Results
At recurrence, 31.4 % were treated with curative-intent treatments (surgery or ablation), 42.1 % received palliative treatment, and 26.4 % received best supportive care. The 1-, 3-, and 5-year survivals, respectively, after HCC recurrence were 75, 60, and 31 %, vs. 60, 19, and 12 %, vs. 52, 4, and 5 % (p < 0.001). By multivariate analysis, not being amenable to a curative-intent treatment [hazard ratio (HR) 4.7, 95 % confidence interval (CI) 2.7–8.3, p < 0.001], α-fetoprotein of ≥100 ng/mL at the time of HCC recurrence (HR 2.1, 95 % CI 1.3–2.3, p = 0.002) and early recurrence (<12 months) after LT (HR 1.6, 95 % CI 1.1–2.5, p = 0.03) were found to be poor prognosis factors. A prognostic score was devised on the basis of these three independent variables. Patients were divided into three groups, as follows: good prognosis, 0 points (n = 22); moderate prognosis, 1 or 2 points (n = 84); and poor prognosis, 3 points (n = 15). The 1-, 3-, and 5-year actuarial survival for each group was 91, 50, and 50 %, vs. 52, 7, and 2 %, vs. 13, 0, and 0 %, respectively (p < 0.001).
Conclusions
Patients with HCC recurrence after transplant amenable to curative-intent treatments can experience significant long-term survival (~50 % at 5 years), so aggressive management should be offered. Poor prognosis factors after recurrence are not being amenable to a curative-intent treatment, α-fetoprotein of ≥100 ng/mL, and early (<1 year) recurrence after LT.


Similar content being viewed by others
References
Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;31:1245–55.
Yao FY. Liver transplantation for hepatocellular carcinoma: beyond the Milan criteria. Am J Transplant. 2008;8:1982–9.
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, Camerini T, et al; Metroticket Investigator Study Group. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10:35–43.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–9.
DuBay D, Sandroussi C, Sandhu L, Cleary S, Guba M, Cattral MS, McGilvray I, et al. Liver transplantation for advanced hepatocellular carcinoma using poor tumor differentiation on biopsy as an exclusion criterion. Ann Surg. 2011;253:166–72.
Jonas S, Bechstein WO, Steinmüller T, Herrmann M, Radke C, Berg T, Settmacher U, et al. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology. 2001;33:1080–6.
Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20:325–39.
Cillo U, Vitale A, Grigoletto F, Gringeri E, D’Amico F, Valmasoni M, Brolese A, et al. Intention-to-treat analysis of liver transplantation in selected, aggressively treated HCC patients exceeding the Milan criteria. Am J Transpl. 2007;7:972–81.
Toso C, Cader S, Mentha-Dugerdil A, Meeberg G, Majno P, Morard I, Giostra E, et al. Factors predicting survival after post-transplant hepatocellular carcinoma recurrence. J Hepatobiliary Pancreat Sci. 2013;20:342–7.
Welker MW, Bechstein WO, Zeuzem S, Trojan J. Recurrent hepatocellular carcinoma after liver transplantation—an emerging clinical challenge. Transpl Int. 2013;26:109–18.
DuBay DA, Sandroussi C, Kachura JR, Ho CS, Beecroft JR, Vollmer CM, Ghanekar A, et al. Radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. HPB (Oxford). 2011;13:24–32.
Wo JY, Dawson LA, Zhu AX, Hong TS. An emerging role for radiation therapy in the treatment of hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Surg Oncol Clin N Am. 2014;23:353–68.
Sapisochin G, Castells L, Dopazo C, Bilbao I, Minguez B, Lázaro JL, Allende H, et al. Single HCC in cirrhotic patients: liver resection or liver transplantation? Long-term outcome according to an intention-to-treat basis. Ann Surg Oncol. 2013;20:1194–202.
Valdivieso A, Bustamante J, Gastaca M, Uriarte JG, Ventoso A, Ruiz P, Fernandez JR, et al. Management of hepatocellular carcinoma recurrence after liver transplantation. Transpl Proc. 2010;42:660–2.
Pfiffer TE, Seehofer D, Nicolaou A, Neuhaus R, Riess H, Trappe RU. Recurrent hepatocellular carcinoma in liver transplant recipients: parameters affecting time to recurrence, treatment options and survival in the sorafenib era. Tumori. 2011;97:436–41.
Taketomi A, Toshima T, Kitagawa D, Motomura T, Takeishi K, Mano Y, Kayashima H, et al. Predictors of extrahepatic recurrence after curative hepatectomy for hepatocellular carcinoma. Ann Surg Oncol. 2010;17:2740–6.
Toso C, Mentha G, Majno P. Integrating sorafenib into an algorithm for the management of post-transplant hepatocellular carcinoma recurrence. J Hepatol. 2013;59:3–5.
Kornberg A, Küpper B, Tannapfel A, Katenkamp K, Thrum K, Habrecht O, Willberg J. Long-term survival after recurrent hepatocellular carcinoma in liver transplant patients: clinical patterns and outcome variables. Eur J Surg Oncol. 2010;36:275–80.
Roayaie S, Schwartz JD, Sung MW, Emre SH, Miller CM, Gondolesi GE, Krieger NR, et al. Recurrence of hepatocellular carcinoma after liver transplant: patterns and prognosis. Liver Transpl. 2004;10:534–44.
Hameed B, Mehta N, Sapisochin G, Roberts JP, Yao FY. Alpha-fetoprotein >1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting Milan criteria. Liver Transpl. 2014.
Duvoux C, Roudot-Thoraval F, Decaens T, Pessione F, Badran H, Piardi T, Francoz C, et al; Liver Transplantation French Study Group. Liver transplantation for hepatocellular carcinoma: a model including α-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012;143:986–94.
Shah SA, Cleary SP, Wei AC, Yang I, Taylor BR, Hemming AW, Langer B, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery. 2007;141:330–9.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sapisochin, G., Goldaracena, N., Astete, S. et al. Benefit of Treating Hepatocellular Carcinoma Recurrence after Liver Transplantation and Analysis of Prognostic Factors for Survival in a Large Euro-American Series. Ann Surg Oncol 22, 2286–2294 (2015). https://doi.org/10.1245/s10434-014-4273-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4273-6