Abstract
Introduction
Peripheral neuropathies (PNPs) encompass a large group of disorders of heterogeneous origin which can manifest themselves with sensory and/or motor deficits depending on the predominantly affected nerve fiber modality. It represents a highly prevalent disease group which can be associated with significant disability and poor recovery. Exercise has the potential to improve side effects of PNP.
Objective
Our objective in this systematic review was to analyze exercise interventions for neuropathic patients in order to evaluate the possible benefits of exercise.
Methods
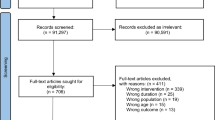
Three independent reviewers used PubMed, MEDPILOT® (MEDLINE), Cochrane, and relevant reference lists to obtain the data. Relevant studies were graded according to the Oxford Levels of Evidence.
Results
Eighteen studies (ten randomized controlled trials and eight controlled clinical trials) met all inclusion criteria. Three (diabetic) studies were ranked very high quality [1b (A)], nine high quality (four diabetes, one cancer, four others) [2b (B)], while six (four diabetes, two others) showed low quality (4/C). Current data suggests that exercise is a feasible, safe, and promising supportive measure for neuropathic patients. This is best documented for patients with diabetic peripheral neuropathy (DPN), suggesting that endurance training has the potential to prevent the onset of and reduce the progression of DPN. In general, balance exercises showed the highest effect on the motor as well as sensory symptoms in all types of PNP.
Conclusion
Overall, balance training appears to be the most effective exercise intervention. Studies focusing exclusively on strength, or a combination of endurance and strength, appear to have a lower impact. For metabolically-induced neuropathies, endurance training also plays an important role. Further research with high methodological quality needs to be conducted in order to establish evidence-based clinical recommendations for neuropathic patients.

Similar content being viewed by others
References
Martyn CN, Hughes RA. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62(4):310–8.
Mold JW, Vesely SK, Keyl BA, et al. The prevalence, predictors, and consequences of peripheral sensory neuropathy in older patients. J Am Board Fam Pract. 2004;17(5):309–18.
Richardson JK, Ashton-Miller JA. Peripheral neuropathy: an often-overlooked cause of falls in the elderly. Postgraduate Med. 1996;99(6):161–72.
Lee K, Lee S, Song C. Whole-body vibration training improves balance, muscle strength and glycosylated hemoglobin in elderly patients with diabetic neuropathy. Tohoku J Exp Med. 2013;231(4):305–14.
Liedberg GM, Vrethem M. Polyneuropathy, with and without neurogenic pain, and its impact on daily life activities: a descriptive study. Disabil Rehabil. 2009;31(17):1402–8. doi:10.1080/09638280802621382.
Stubblefield MD, Burstein HJ, Burton AW, et al. NCCN task force report: management of neuropathy in cancer. J Natl Compre Canc Netw. 2009;7 Suppl 5:S1–S26; quiz S7–8.
Poeck K, Hacke W. Neurologie. Springer; 2006.
Sartor CD, Watari R, Passaro AC, et al. Effects of a combined strengthening, stretching and functional training program versus usual-care on gait biomechanics and foot function for diabetic neuropathy: a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:36. doi:10.1186/1471-2474-13-36.
Boulton AJ. Lowering the risk of neuropathy, foot ulcers and amputations. Diabet Med. 1998;15(Suppl 4):S57–9. doi:10.1002/(SICI)1096-9136(1998120)15:4+<S57:AID-DIA741>3.0.CO;2-D.
Quasthoff S, Hartung HP. Chemotherapy-induced peripheral neuropathy. J Neurol. 2002;249(1):9–17.
Antoine JC, Camdessanche JP. Peripheral nervous system involvement in patients with cancer. Lancet Neurol. 2007;6(1):75–86. doi:10.1016/S1474-4422(06)70679-2.
Kaley TJ, Deangelis LM. Therapy of chemotherapy-induced peripheral neuropathy. Br J Haematol. 2009;145(1):3–14. doi:10.1111/j.1365-2141.2008.07558.x.
Wonders KY, Reigle BS, Drury DG. Treatment strategies for chemotherapy-induced peripheral neuropathy: potential role of exercise. Oncol Rev. 2010;4:117–25.
Tofthagen C, Visovsky C, Berry DL. Strength and balance training for adults with peripheral neuropathy and high risk of fall: current evidence and implications for future research. Oncol Nurs Forum. 2012;39(5):E416–24. doi:10.1188/12.ONF.E416-E424.
Uceyler N, Rogausch JP, Toyka KV, et al. Differential expression of cytokines in painful and painless neuropathies. Neurology. 2007;69(1):42–9. doi:10.1212/01.wnl.0000265062.92340.a5.
Smith EM, Cohen JA, Pett MA, et al. The reliability and validity of a modified total neuropathy score-reduced and neuropathic pain severity items when used to measure chemotherapy-induced peripheral neuropathy in patients receiving taxanes and platinums. Cancer Nurs. 2010;33(3):173–83. doi:10.1097/NCC.0b013e3181c989a3.
Smith BH, Torrance N, Bennett MI, et al. Health and quality of life associated with chronic pain of predominantly neuropathic origin in the community. Clin J Pain. 2007;23(2):143–9. doi:10.1097/01.ajp.0000210956.31997.89.
Granacher U, Muehlbauer T, Gollhofer A, et al. An intergenerational approach in the promotion of balance and strength for fall prevention: a mini-review. Gerontology. 2011;57(4):304–15. doi:10.1159/000320250.
Bruhn S, Kullmann N, Gollhofer A. The effects of a sensorimotor training and a strength training on postural stabilisation, maximum isometric contraction and jump performance. Int J Sports Med. 2004;25(1):56–60. doi:10.1055/s-2003-45228.
Balducci S, Leonetti F, Di Mario U, et al. Is a long-term aerobic plus resistance training program feasible for and effective on metabolic profiles in type 2 diabetic patients? Diabetes Care. 2004;27(3):841–2.
Goldhaber-Fiebert JD, Goldhaber-Fiebert SN, Tristan ML, et al. Randomized controlled community-based nutrition and exercise intervention improves glycemia and cardiovascular risk factors in type 2 diabetic patients in rural Costa Rica. Diabetes Care. 2003;26(1):24–9.
Balducci S, Iacobellis G, Parisic L, et al. Exercise training can modify the natural history of diabetic peripheral neuropathy. J Diabet Complicat. 2006;20:216–23.
Granacher U, Mühlbauer T, Taube W, et al. Sensorimotor training. In: Cardinale M, editor. Strength and conditioning: biological principles and practical applications. San Francisco: Wiley; 2011: p. 399–409.
Kawanabe K, Kawashima A, Sashimoto I, et al. Effect of whole-body vibration exercise and muscle strengthening, balance, and walking exercises on walking ability in the elderly. Keio J Med. 2007;56(1):28–33.
Ahn S, Song R. Effects of Tai Chi Exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. J Altern Complement Med. 2012;18(12):1172–8. doi:10.1089/acm.2011.0690.
Taube W, Gruber M, Beck S, et al. Cortical and spinal adaptations induced by balance training: correlation between stance stability and corticospinal activation. Acta Physiol (Oxf). 2007;189(4):347–58. doi:10.1111/j.1365-201X.2007.01665.x.
Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47(4):678–85.
Taube W, Kullmann N, Leukel C, et al. Differential reflex adaptations following sensorimotor and strength training in young elite athletes. Int J Sports Med. 2007;28(12):999–1005. doi:10.1055/s-2007-964996.
Verhagen E, van der Beek A, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–93. doi:10.1177/0363546503262177.
Granacher U, Gollhofer A, Strass D. Training induced adaptations in characteristics of postural reflexes in elderly men. Gait Posture. 2006;24(4):459–66. doi:10.1016/j.gaitpost.2005.12.007.
Bogaerts A, Delecluse C, Boonen S, et al. Changes in balance, functional performance and fall risk following whole body vibration training and vitamin D supplementation in institutionalized elderly women: a 6 month randomized controlled trial. Gait Posture. 2011;33(3):466–72. doi:10.1016/j.gaitpost.2010.12.027.
Rittweger J, Beller G, Armbrecht G, et al. Prevention of bone loss during 56 days of strict bed rest by side-alternating resistive vibration exercise. Bone. 2010;46(1):137–47. doi:10.1016/j.bone.2009.08.051.
Kirchner E. Pflegerische Interventionen und Möglichkeiten bei krebstherapiebedingter Polyneuropathie. DLH-INFO. 2008;37:19–21.
Blottner D, Salanova M, Puttmann B, et al. Human skeletal muscle structure and function preserved by vibration muscle exercise following 55 days of bed rest. Eur J Appl Physiol. 2006;97(3):261–71. doi:10.1007/s00421-006-0160-6.
Lau RW, Liao LR, Yu F, et al. The effects of whole body vibration therapy on bone mineral density and leg muscle strength in older adults: a systematic review and meta-analysis. Clin Rehabil. 2011;25(11):975–88. doi:10.1177/0269215511405078.
Cochrane DJ. Vibration exercise: the potential benefits. Int J Sports Med. 2011;32(2):75–99. doi:10.1055/s-0030-1268010.
Spiliopoulou SI, Amiridis IG, Tsigganos G, et al. Vibration effects on static balance and strength. Int J Sports Med. 2010;31(9):610–6. doi:10.1055/s-0030-1249618.
Jacobson B, Chen H, Cashel C. The effect of Tai Chi Chuan training on balance, kinesthetic sense and strength. Percept Mot Skills. 1997;84:27–33.
Harmer PA, Li F. Tai Chi and falls prevention in older people. Med Sport Sci. 2008;52:124–34. doi:10.1159/000134293.
Lan C, Lai JS, Chen SY, et al. 12-month Tai Chi training in the elderly: its effect on health fitness. Med Sci Sports Exerc. 1998;30(3):345–51.
Richerson S, Rosendale K. Does Tai Chi improve plantar sensory ability? A pilot study. Diabetes Technol Ther. 2007;9(3):276–86. doi:10.1089/dia.2006.0033.
Wolfson L, Whipple R, Derby C, et al. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am Geriatr Soc. 1996;44(5):498–506.
Wong AM, Lin YC, Chou SW, et al. Coordination exercise and postural stability in elderly people: Effect of Tai Chi Chuan. Arch Phys Med Rehabil. 2001;82(5):608–12. doi:10.1053/apmr.2001.22615.
Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Appl Nurs Res. 2002;15(4):235–42. doi:10.1053/apnr.2002.35975.
Li F, Harmer P, McAuley E, et al. An evaluation of the effects of Tai Chi exercise on physical function among older persons: a randomized controlled trial. Ann Behav Med. 2001;23(2):139–46.
Atkins D, Eccles M, Flottorp S, et al. Systems for grading the quality of evidence and the strength of recommendations. I: critical appraisal of existing approaches. The GRADE Working Group. BMC Health Serv Res. 2004;4(1):38. doi:10.1186/1472-6963-4-38.
Baumann FT, Zopf EM, Bloch W. Clinical exercise interventions in prostate cancer patients: a systematic review of randomized controlled trials. Support Care Cancer. 2012;20(2):221–33. doi:10.1007/s00520-011-1271-0.
Mac Dermid J, Law M. Evaluating the evidence. In: Law MC MacDermid J, editor. Evidence-based rehabilitation: a guide to practise. Thorofare: SLACK Incorporated; 2008. p. 122.
Bicego D, Brown K, Ruddick M, et al. Effects of exercise on quality of life in women living with breast cancer: a systematic review. Breast J. 2009;15(1):45–51. doi:10.1111/j.1524-4741.2008.00670.x.
Weis J, Domann U. Interventions in the rehabilitation of breast cancer patients: a critical literature review of the state of the art. Die Rehabil. 2006;45(3):129–45. doi:10.1055/s-2005-915459.
Philipps B, Ball C, Sackett D, et al. Oxford Centre for Evidence-based Medicine-Levels of evidence. March 2009. Available from: http://www.cebm.net/index.aspx?o=1025. 2014.
Dixit S, Maiya AG, Shastry BA. Effect of aerobic exercise on peripheral nerve functions of population with diabetic peripheral neuropathy in type 2 diabetes: a single blind, parallel group randomized controlled trial. J Diabet Complicat. 2013;28(3):332–9. doi:10.1016/j.jdiacomp.2013.12.006.
Mueller MJ, Tuttle LJ, Lemaster JW, et al. Weight-bearing versus nonweight-bearing exercise for persons with diabetes and peripheral neuropathy: a randomized controlled trial. Arch Phys Med Rehabil. 2013;94(5):829–38. doi:10.1016/j.apmr.2012.12.015.
Akbari M, Jafari H, Moshashaee A, et al. Do diabetic neuropathy patients benefit from balance training? J Rehabil Res Dev. 2012;49(2):333–8.
Song CH, Petrofsky JS, Lee SW, et al. Effects of an exercise program on balance and trunk proprioception in older adults with diabetic neuropathies. Diabet Technol Ther. 2011;13(8):803–11.
Allet L, Armand S, de Bie RA, et al. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia. 2010;53(3):458–66. doi:10.1007/s00125-009-1592-4.
Hung JW, Liou CW, Wang PW, et al. Effect of 12-week tai chi chuan exercise on peripheral nerve modulation in patients with type 2 diabetes mellitus. J Rehabil Med. 2009;41(11):924–9. doi:10.2340/16501977-0445.
Kruse RL, Lemaster JW, Madsen RW. Fall and balance outcomes after an intervention to promote leg strength, balance, and walking in people with diabetic peripheral neuropathy: “feet first” randomized controlled trial. Phys Ther. 2010;90(11):1568–79. doi:10.2522/ptj.20090362.
Richardson JK, Sandman D, Vela S. A focused exercise regimen improves clinical measures of balance in patients with peripheral neuropathy. Arch Phys Med Rehabil. 2001;82(2):205–9.
Streckmann F, Kneis S, Leifert JA, et al. Exercise program improves therapy-related side-effects and quality of life in lymphoma patients undergoing therapy. Ann Oncol. 2014;25(2):493–9. doi:10.1093/annonc/mdt568.
Matjacic Z, Zupan A. Effects of dynamic balance training during standing and stepping in patients with hereditary sensory motor neuropathy. Disabil Rehabil. 2006;28(23):1455–9. doi:10.1080/09638280600646169.
Tomás MT, Santa-Clara H, Bruno PM, et al. The impact of exercise training on liver transplanted familial amyloidotic polyneuropathy (FAP) patients. Transplantation. 2013;95(2):372–7. doi:10.1097/TP.0b013e31827220e7.
Graham RC, Hughes RA, White CM. A prospective study of physiotherapist prescribed community based exercise in inflammatory peripheral neuropathy. J Neurol. 2007;254(2):228–35. doi:10.1007/s00415-006-0335-4.
Nardone A, Godi M, Artuso A, et al. Balance rehabilitation by moving platform and exercises in patients with neuropathy or vestibular deficit. Arch Phys Med Rehabil. 2010;91(12):1869–77. doi:10.1016/j.apmr.2010.09.011.
Ruhland JL, Shields RK. The effects of a home exercise program on impairment and health-related quality of life in persons with chronic peripheral neuropathies. Phys Ther. 1997;77(10):1026–39.
Lindeman E, Leffers P, Spaans F, et al. Strength training in patients with myotonic dystrophy and hereditary motor and sensory neuropathy: a randomized clinical trial. Arch Phys Med Rehabil. 1995;76(7):612–20.
Ang CD, Alviar MJ, Dans AL, et al. Vitamin B for treating peripheral neuropathy. Cochrane Database Syst Rev. 2008;(3):CD004573. doi:10.1002/14651858.CD004573.pub3.
Albers JW, Chaudhry V, Cavaletti G, et al. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database Syst Rev. 2014;(3):CD005228. doi:10.1002/14651858.CD005228.pub4.
Apfel SC. Nerve growth factor for the treatment of diabetic neuropathy: what went wrong, what went right, and what does the future hold? Int Rev Neurobiol. 2002;50:393–413.
American Diabetes Assocation. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37 Suppl 1:S14–80. doi:10.2337/dc14-S014.
Tolle T, Xu X, Sadosky AB. Painful diabetic neuropathy: a cross-sectional survey of health state impairment and treatment patterns. J Diabet Complicat. 2006;20(1):26–33. doi:10.1016/j.jdiacomp.2005.09.007.
Possidente CJ, Tandan R. A survey of treatment practices in diabetic peripheral neuropathy. Prim Care Diabet. 2009;3(4):253–7. doi:10.1016/j.pcd.2009.08.008.
Kessler NJ, Hong J. Whole body vibration therapy for painful diabetic peripheral neuropathy: a pilot study. J Bodyw Mov Ther. 2013;17(4):518–22. doi:10.1016/j.jbmt.2013.03.001.
Albers JW, Chaudhry V, Cavaletti G, et al. Interventions for preventing neuropathy caused by cisplatin and related compounds. Cochrane Database Syst Rev. 2011;(2):CD005228. doi:10.1002/14651858.CD005228.pub3.
Steimann M, Kerschgens C, Barth J. Rehabilitation bei Chemotherapieinduzierter Polyneuropathie. Onkologe. 2011;17:940–7.
Sabatier MJ, Redmon N, Schwartz G, et al. Treadmill training promotes axon regeneration in injured peripheral nerves. Exp Neurol. 2008;211(2):489–93. doi:10.1016/j.expneurol.2008.02.013.
Molteni R, Zheng JQ, Ying Z, et al. Voluntary exercise increases axonal regeneration from sensory neurons. Proc Natl Acad Sci U S A. 2004;101(22):8473–8. doi:10.1073/pnas.0401443101.
Park JS, Hoke A. Treadmill exercise induced functional recovery after peripheral nerve repair is associated with increased levels of neurotrophic factors. PloS One. 2014;9(3):e90245. doi:10.1371/journal.pone.0090245.
Tomlinson DR, Gardiner NJ. Glucose neurotoxicity. Nat Rev Neurosci. 2008;9(1):36–45. doi:10.1038/nrn2294.
Kikkawa Y, Kuwabara S, Misawa S, et al. The acute effects of glycemic control on nerve conduction in human diabetics. Clin Neurophysiol. 2005;116(2):270–4. doi:10.1016/j.clinph.2004.08.011.
Lee Y, Morrison BM, Li Y, et al. Oligodendroglia metabolically support axons and contribute to neurodegeneration. Nature. 2012;487(7408):443–8. doi:10.1038/nature11314.
Quistorff B, Secher NH, Van Lieshout JJ. Lactate fuels the human brain during exercise. FASEB J. 2008;22(10):3443–9. doi:10.1096/fj.08-106104.
Taube W, Gruber M, Gollhofer A. Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiologica. 2008;193(2):101–16. doi:10.1111/j.1748-1716.2008.01850.x.
Gollhofer A. Proprioceptive training: considerations for strength and power production. In: P.V.K, editor. Strength and power in sport. 2nd ed. Oxford: Blackwell Publishing; 2003. p. 331–42.
Sjostrom PJ, Rancz EA, Roth A, Hausser M. Dendritic excitability and synaptic plasticity. Physiol Rev. 2008;88(2):769–840. doi:10.1152/physrev.00016.2007.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328(7454):1490. doi:10.1136/bmj.328.7454.1490.
Segal RJ, Reid RD, Courneya KS, et al. Randomized controlled trial of resistance or aerobic exercise in men receiving radiation therapy for prostate cancer. J Clin Oncol. 2009;27(3):344–51. doi:10.1200/JCO.2007.15.4963.
ADA. 2014. www.diabetes.org. Accessed 3 Oct 2014.
Acknowledgments
Fiona Streckmann, Eva M. Zopf, Helmar C. Lehmann, Kathrin May, Julia Rizza, Philipp Zimmer, Albert Gollhofer, Wilhelm Bloch, and Freerk T. Baumann have no conflicts of interest to declare. No sources of funding were used to assist in the preparation of this manuscript. We acknowledge the advisory support of C. Brinkmann.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Streckmann, F., Zopf, E.M., Lehmann, H.C. et al. Exercise Intervention Studies in Patients with Peripheral Neuropathy: A Systematic Review. Sports Med 44, 1289–1304 (2014). https://doi.org/10.1007/s40279-014-0207-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-014-0207-5