Opinion Statement
Benefits of liver transplantation (LT) for patients with hepatocellular carcinoma (HCC) are well established. However, there is debate regarding optimal and equitable selection of patients best served by LT, particularly in the face of limited organ availability. Herein, we discuss topics regarding LT selection criteria for patients with HCC. Recent change in UNOS policy currently mandates a 6-month observation period prior to priority listing and institutes a cap of 34 MELD exception points for patients with HCC. Additionally, two further proposed changes to UNOS policy include (1) requiring locoregional therapy for those with small (2–3 cm) unifocal HCC prior to applying for exception points and (2) allowing downstaging in select patients with UNOS T3 lesions. These policies move beyond simply using tumor burden to using markers of tumor biology for selecting patients who have the lowest risk of post-transplant recurrence and best chance at long-term post-transplant survival. Given increasing time on transplant waiting lists and shortage of donor grafts, LT should be reserved for patients who may achieve significant benefit compared to non-transplant therapies. Potential benefit to HCC patients must be weighed against the harm from delaying or precluding LT for non-HCC patients on the waiting list, particularly in regions with limited donor availability. The relative benefit of LT in patients with small (<3 cm) HCC is likely limited; surgical resection (in absence of portal hypertension) and local ablative therapy (if portal hypertension present) are both efficacious and more cost-effective and should likely be regarded as first line therapies for these patients. Salvage LT can be considered as a rescue option for those with recurrent disease. Downstaging for selected patients with UNOS T3 lesions may identify those with good tumor biology and acceptable post-transplant outcomes; however, current studies have had a wide variation in reported outcomes. While awaiting more data, a standardized downstaging protocol including a priori inclusion criteria and a mandatory waiting time prior to LT to observe tumor biology likely yields the best outcomes.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
El-Serag HB. Hepatocellular Carcinoma. N Engl J Med. 2011;365(12):1118–27.
Mazzaferro V, Bhoori S, Sposito C, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transpl. 2011;17(Suppl 2):S44–57.
•• Heimbach JK, Hirose R, Stock PG, et al. Delayed hepatocellular carcinoma model for end-stage liver disease exception score improves disparity in access to liver transplant in the United States. Hepatology. 2015;61(5):1643–50. Authors demonstrated a 6–9-month delay in receipt of MELD exception points reduces disparity in transplant rates between HCC and non-HCC candidates.
Sotiropoulos GC, Molmenti EP, Losch C, et al. Meta-analysis of tumor recurrence after liver transplantation for hepatocellular carcinoma based on 1,198 cases. Eur J Med Res. 2007;12(10):527–34.
Halazun KJ, Patzer RE, Rana AA, et al. Standing the test of time: outcomes of a decade of prioritizing patients with hepatocellular carcinoma, results of the UNOS natural geographic experiment. Hepatology. 2014;60(6):1957–62.
• Mehta N, Heimbach J, Harnois DM, et al. Short waiting time predicts early recurrence of hepatocellular carcinoma after liver transplantation: a multicenter study supporting the “ablate and wait” principle. Paper presented at: The Liver Meeting 2014; Boston, MA. Multi-center study demonstrated liver transplant waiting times less than 6 months is predictive of post-transplant recurrence of hepatocellular carcinoma.
Wang JH, Wang CC, Hung CH, et al. Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J Hepatol. 2012;56(2):412–8.
Hung HH, Chiou YY, Hsia CY, et al. Survival rates are comparable after radiofrequency ablation or surgery in patients with small hepatocellular carcinomas. Clin Gastroenterol Hepatol. 2011;9(1):79–86.
Naugler WE, Sonnenberg A. Survival and cost-effectiveness analysis of competing strategies in the management of small hepatocellular carcinoma. Liver Transpl. 2010;16(10):1186–94.
• Mehta N, Sarkar M, Dodge JL, Fidelman N, Roberts JP, Yao FY. Intention-to-treat outcome of T1 hepatocellular carcinoma with the “wait and not ablate” approach until meeting T2 criteria for liver transplant listing. Liver Transpl. 2016;22(2):178–87. The risk of tumor progression from T1 directly to beyond T2 is low (< 5%) within 6 months, although the ideal strategy in these patients (immediate ablation vs. watchful waiting) remains unknown.
Nathan H, Segev DL, Mayo SC, et al. National trends in surgical procedures for hepatocellular carcinoma: 1998-2008. Cancer. 2012;118(7):1838–44.
Zheng Z, Liang W, Milgrom DP, et al. Liver transplantation versus liver resection in the treatment of hepatocellular carcinoma: a meta-analysis of observational studies. Transplantation. 2014;97(2):227–34.
• Vitale A, Huo TL, Cucchetti A, et al. Survival benefit of liver transplantation versus resection for hepatocellular carcinoma: impact of MELD score. Ann Surg Oncol. 2015;22(6):1901–7. Surgical resection is the cost effective approach to HCC patients with compensated cirrhosis if MELD score is below 10 and there is no evidence of microvascular invasion.
Cho YK, Kim JK, Kim MY, et al. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology (Baltimore, Md). 2009;49(2):453–9.
Zheng SS, Xu X, Wu J, et al. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 2008;85(12):1726–32.
Guiteau JJ, Cotton RT, Washburn WK, et al. An early regional experience with expansion of Milan criteria for liver transplant recipients. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2010;10(9):2092–8.
Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33(6):1394–403.
Freeman RB, Mithoefer A, Ruthazer R, et al. Optimizing staging for hepatocellular carcinoma before liver transplantation: a retrospective analysis of the UNOS/OPTN database. Liver Transpl. 2006;12(10):1504–11.
Duffy JP, Vardanian A, Benjamin E, et al. Liver transplantation criteria for hepatocellular carcinoma should be expanded: a 22-year experience with 467 patients at UCLA. Ann Surg. 2007;246(3):502–9. discussion 509-511
Xu X, Lu D, Ling Q, et al. Liver transplantation for hepatocellular carcinoma beyond the Milan criteria. Gut. 2016;65(6):1035–41.
Kim PT, Onaca N, Chinnakotla S, et al. Tumor biology and pre-transplant locoregional treatments determine outcomes in patients with T3 hepatocellular carcinoma undergoing liver transplantation. Clin Transpl. 2013;27(2):311–8.
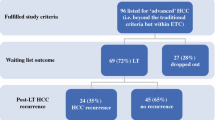
Sapisochin G, Goldaracena N, Laurence JM, et al. The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: a prospective validation study. Hepatology. 2016;64(6):2077–88.
Yao FY, Mehta N, Flemming J, et al. Downstaging of hepatocellular cancer before liver transplant: long-term outcome compared to tumors within Milan criteria. Hepatology. 2015;61(6):1968–77.
Mehta N, Guy J, Frenette CT, et al. Multicenter Study of Down-staging of hepatocellular carcinoma (HCC) to within Milan criteria before liver transplantation (LT). Paper presented at: The Liver Meeting Boston, MA; 2014
• Parikh ND, Waljee AK, Singal AG. Downstaging hepatocellular carcinoma: a systematic review and pooled analysis. Liver Transpl. 2015;21(9):1142–52. There is variation in post-transplant recurrence rates and post-transplant survival with downstaging, although a priori inclusion criteria, mandatory waiting time prior to transplantation, and a standardized downstaging protocol are the approaches that likely yield the best outcomes.
Volk ML, Vijan S, Marrero JA. A novel model measuring the harm of transplanting hepatocellular carcinoma exceeding Milan criteria. Am J Transplant. 2008;8(4):839–46.
Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10(1):35–43.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nicole Rich and Neehar D. Parikh declare that they have no conflict of interest.
Amit G. Singal reports personal fees from Bayer, Eisai, EMD Serano, and Wako Diagnostics but none are directly relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Liver
Rights and permissions
About this article
Cite this article
Rich, N.E., Parikh, N.D. & Singal, A.G. Hepatocellular Carcinoma and Liver Transplantation: Changing Patterns and Practices. Curr Treat Options Gastro 15, 296–304 (2017). https://doi.org/10.1007/s11938-017-0133-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11938-017-0133-3