Abstract
Goals of work
Comparing antiemetic efficacy of different 5-HT3-receptor antagonists (5-HT3RAs) is difficult due to inter-study variability. Therefore, a meta-analysis was performed to comparatively evaluate dolasetron, granisetron, ondansetron and tropisetron for acute chemotherapy-induced nausea and vomiting (CINV).
Patients and methods
Comparisons between 5-HT3RAs were based on 44 randomized studies (including 12,343 patients) identified by MEDLINE, CANCERLIT or EMBASE searches and subcategorized by chemotherapy type (cisplatin- or non-cisplatin-based).
Main results
When all studies were combined, granisetron was equivalent to ondansetron (n = 27), and showed an advantage vs tropisetron (p = 0.018; n = 12). Ondansetron vs tropisetron (n = 11) and ondansetron vs dolasetron (n = 3) revealed equivalence in each comparison. An advantage for 3 mg granisetron vs 8 mg ondansetron was found in non-cisplatin-based studies (p = 0.015; n = 6). Overall equivalence was seen between ondansetron, 24 or 32 mg, and granisetron, 2 or 3 mg, for all studies (n = 13). There was a possible advantage for higher (24 or 32 mg) vs lower (8 mg) ondansetron dose regimens with cisplatin-based trials (n = 6). No differences were seen between 3 and 1 mg granisetron doses (n = 6).
Conclusions
Efficacy of 5-HT3RAs for preventing CINV following cisplatin- and non-cisplatin-based chemotherapy is comparable, with the exception of granisetron vs tropisetron. Some differences were noted in dosing subanalyses.
Similar content being viewed by others
Introduction
Nausea and vomiting are distressing and debilitating side-effects of chemotherapy and radiotherapy, which if left untreated may result in physiological changes including dehydration, electrolyte imbalance and malnutrition [36]. These adverse events may impact on patients’ quality of life, hinder compliance with cancer treatment and potentially compromise treatment outcome [26]. Chemotherapy-induced nausea and vomiting (CINV) commonly occur within a few hours of treatment and may continue for several days. Symptoms are therefore classified as acute (<24 h post-chemotherapy) or delayed (>24 h post-chemotherapy). The onset and duration of nausea and vomiting do, however, vary depending on which chemotherapy agents are used.
A number of antiemetic agents are available for the management of nausea and vomiting, including 5-HT3-receptor antagonists, corticosteroids, NK1 receptor antagonists, dopamine-receptor antagonists, neuroleptics and benzodiazepines. 5-HT3-receptor antagonists are currently recommended for prophylaxis of nausea and vomiting associated with highly and moderately emetogenic chemotherapy [47]. Studies directly comparing the efficacy of different 5-HT3-receptor antagonists have failed to demonstrate clear superiority of any one agent; however, differences in their receptor specificities and pharmacological profiles may have an impact on their clinical efficacy over the full 24-h acute period [31].
To date, published studies have shown conflicting results. Large studies have shown heterogeneous results, while results of small studies need to be interpreted with caution due to lack of power or differences in trial designs and patient populations. A comprehensive meta-analysis of trials is therefore required to clarify overall outcomes. Few systematic reviews that compare the efficacy of the 5-HT3-receptor antagonists in the management of acute CINV have been completed, and none has clearly demonstrated superiority of one agent over another. These studies include a comparison of granisetron (Kytril®, Hoffmann-La Roche, Nutley, NJ, USA), ondansetron (Zofran®, GlaxoSmithKline, Research Triangle Park, NC, USA), tropisetron (Navoban®, Novartis Pharmaceuticals, North Ryde NSW, Australia) and dolasetron (Anzemet®, Aventis Pharmaceuticals, Kansas City, MO, USA), using all studies as references rather than head-to-head trials [16], and meta-analyses of randomized trials comparing granisetron with ondansetron [13], granisetron or tropisetron with ondansetron [5] and granisetron with ondansetron in high-dose cisplatin-based chemotherapy regimens [45]. One of the reviews is available as an abstract only [5], while one is in Spanish [45], and another is in German [16]. The prospective studies included in the latter publication were deemed too small to conclude whether one agent was more effective than another, and the retrospective analysis was designed to look for the optimal antiemetic treatment regimen for acute and delayed emesis, rather than comparing the 5-HT3-receptor antagonists. Importantly, none of the above reviews or meta-analyses included a comparison of all the commonly available 5-HT3-receptor antagonists.
This paper presents a meta-analysis of randomized trials of four currently available 5-HT3-receptor antagonists—dolasetron, granisetron, ondansetron and tropisetron—to attempt to clarify differences in their efficacy for prophylaxis of acute CINV. Palonosetron, a new 5-HT3-receptor antagonist with a prolonged half-life was only touched on, as the current paucity of comparative trials does not warrant a formal meta-analysis. More than half of the studies included in this meta-analysis compared granisetron with ondansetron and tested various dosing schedules in conjunction with different chemotherapy regimens. This prompted further sub-studies and dosing analyses for these two antiemetics in the acute phase.
Patients and methods
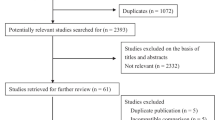
The meta-analysis was performed on the results of 44 randomized studies, including 12,343 patients, comprising direct comparisons between different 5-HT3-receptor antagonists in the treatment of acute CINV [2, 4, 6, 7, 10, 11, 18–20, 22–25, 27–29, 32, 33, 37–44, 46, 48–50, 52, 53, 55–61, 64, 65, 67, 69, 71]. The studies were identified by literature research on English language and non-English language publications referenced in MEDLINE, CANCERLIT or EMBASE and were categorized as follows: granisetron vs ondansetron, granisetron vs tropisetron, ondansetron vs tropisetron and ondansetron vs dolasetron. The trials and publications included had to fulfil the following selection criteria: treatment allocation randomization; parallel-group or crossover design (if response to the first cycle was reported or could be derived); no high-dose chemotherapy requiring blood cell transplantation; insufficient data for evaluation of acute antiemetic efficacy (e.g. only overall data for day 1 to 5 emesis provided); English, French, or German language (at least abstract). If the same trial was published repeatedly, the most recent or most detailed report was selected. Specific dose ranges were prospectively defined for inclusion in the dose-related analyses.
Studies were also subcategorized by the type of chemotherapy received by the patient, i.e. cisplatin-based or non-cisplatin-based. In the cases of a ‘mixed’ chemotherapy-regimen population, without results presented separately according to chemotherapy, the study was categorized according to the predominant cytostatic treatment administered by numbers of patients treated.
Antiemetic efficacy was defined as ‘complete acute response’, i.e. no nausea and vomiting, or only mild nausea within the first 24 h after chemotherapy (as defined by Smith [62] and Soukop [63]) or simply a complete absence of vomiting in the first 24 h after administration of chemotherapy (in cases of insufficient data to apply the nausea criterion).
Response rates were based on individual patients, i.e. the unit of observation taken from the publications for this meta-analysis was the ‘randomized patient’, taking into account data from the first chemotherapy cycle only, whenever possible. Pooled odds ratios were generated separately for cisplatin-based and non-cisplatin-based studies. Combined odds ratios were generated using Mantel-Haenszel pooling of contingency tables (fixed effect model as the standard approach) [68, 70]. In addition, a test for heterogeneity was performed for each combined analysis; a low p value indicates considerable variability between the results of the individual trials, more than would be expected due to chance. In these cases, the pooled therapy group comparison should be considered with care, as the treatment effect might differ with respect to patient selection, drug administration schedules and other factors varying from trial to trial. Thus, random-effects-model results were additionally presented in some of the analyses, as this approach yields more conservative statistical parameters (i.e. confidence intervals and p values) [68]. The figures provide odds ratios with 95% confidence intervals.
The following software was applied for the analyses: TESTIMATE (idv, Gauting, Germany); Comprehensive Meta-Analysis (Biostat, Englewood, NJ, USA).
Results
Granisetron vs ondansetron
Comparisons were made for: granisetron vs ondansetron (all doses), granisetron vs low-dose ondansetron, granisetron vs high-dose ondansetron, and granisetron vs ondansetron excluding dexamethasone. A total of 27 studies comparing all doses of granisetron with all doses of ondansetron were included in the meta-analysis (Table 1) [4, 7, 10, 11, 19, 20, 22, 23, 25, 27, 29, 38–40, 43, 44, 48, 49, 52, 53, 55, 57, 60, 64, 65, 69]. They comprised 16 cisplatin-based studies and 11 non-cisplatin-based studies. Overall pooled odds ratios (including all dose schedules) revealed an overall equivalence of both drugs (Fig. 1).
Subanalyses
Low-dose ondansetron, 8 mg i.v., vs granisetron, 3 mg
A subanalysis of six studies comparing low-dose ondansetron, 8 mg i.v., with granisetron, 3 mg i.v., showed a possible advantage for granisetron in non-cisplatin-based studies (p = 0.015, fixed effect model; Fig. 3b) [27, 29, 43, 53, 60, 69]. However, the latter finding is based on three trials with a total of 183 patients only, showing results with considerable variation (test of heterogeneity: p = 0.041; test of difference, random effects model: p = 0.27).
Comparison of a granisetron, 3 mg (or 40 μg/kg) vs granisetron, 1 mg (or 10 μg/kg) (odds ratios) with cisplatin based chemoteraphy studies and b granisetron, 2/3 mg, vs ondansetron, 24/32 mg, with cisplatin- and non-cisplatin-based chemotherapy studies. An odds ratio (OR) above 1 indicates superiority of ondansetron. *p < 0.05; **p < 0.01
High-dose ondansetron, 24 or 32 mg, vs granisetron, 2 or 3 mg
Thirteen studies comparing higher-dose ondansetron (24 or 32 mg) with granisetron (2 or 3 mg), administered orally or intravenously, revealed an overall equivalence of these doses for both cisplatin-based and non-cisplatin-based studies (Fig. 2b) [4, 7, 10, 11, 22, 38–40, 52, 55, 57, 60, 65]. The results of this subgroup were predominantly driven by two large trials [22, 57], both of which used oral granisetron. Excluding studies using oral antiemetic regimens, seven cisplatin-based studies were compared (n = 1,117); six of these showed a non-significant trend in favour of granisetron (common odds ratio, 0.83; 95% confidence interval, 0.63–1.09), and a high degree of homogeneity between studies was apparent (test for heterogeneity p = 1.0) [4, 39, 40, 52, 55, 60].
Ondansetron was not compared with granisetron, 1 mg, due to a lack of data with this dose.
Granisetron vs ondansetron with the exclusion of dexamethasone
Trials comparing ondansetron with granisetron that did not include administration of dexamethasone were also compared [7, 20, 25, 29, 38–40, 43, 44, 48, 49, 52, 53, 55, 60, 64, 65, 69]. Results showed an overall equivalence of both drugs, similar to the analysis of all the ondansetron vs granisetron studies, some of which included dexamethasone.
Dosing study analyses
Ondansetron, 24 or 32 mg, vs ondansetron, 8 mg
Six cisplatin-based trials were included in this analysis, with ten of the studies identified initially excluded because of lack of randomization or lack of separate reporting of the first cycle in a crossover trial (Table 2) [6, 33, 56, 60, 61, 67]. The fixed-effect model meta-analysis indicates a significant result (p = 0.012) in favour of higher-dose ondansetron regimens (24 or 32 mg; Fig. 3a). However, a highly significant heterogeneity test (p = 0.0023) indicates that the pooled results should be interpreted with caution due to differences between the individual trials. Consequently, a random-effects model was applied and resulted in a higher p value of 0.19.
Granisetron, 1 mg (or 10 μg/kg), vs granisetron, 3 mg (or 40 μg/kg)
Six cisplatin-based trials were included in the comparison of low (1 mg) and high (3 mg) granisetron doses (Table 2), six studies having been excluded due to study design or inadequately reported content [32, 41, 49, 50, 58, 59]. No significant differences in efficacy were seen between the doses (Fig. 2a), and a high degree of homogeneity (test for heterogeneity p = 0.69) was observed between trials.
Granisetron vs tropisetron
The antiemetic efficacy of granisetron was compared with tropisetron in 12 studies (Table 3) [2, 4, 11, 19, 28, 39, 43, 44, 46, 53, 69, 71]. Granisetron was superior to tropisetron (odds ratio > 1.0) in six of the seven cisplatin-based trials, and in four of five non-cisplatin-based studies, although only one of these studies [2] showed a statistically significant benefit of granisetron (Fig. 4a). Pooled analysis of all cisplatin and non-cisplatin-based studies showed a significant advantage in favour of granisetron (p = 0.018), with no major heterogeneity detected (test for heterogeneity p = 0.88).
Ondansetron vs tropisetron
The efficacy of ondansetron and tropisetron was compared in 11 studies (Table 3) [4, 11, 19, 28, 29, 39, 42–44, 53, 69]. Comparisons of these agents in six cisplatin-based studies revealed a non-significant advantage for patients receiving ondansetron compared with tropisetron. However, in non-cisplatin-based studies, a weak trend in the opposite direction was observed. Overall, the differences were neither significant nor of major clinical relevance (Fig. 4b).
Ondansetron vs dolasetron
Only three studies, one cisplatin-based and two non-cisplatin-based, were available for comparisons between ondansetron and dolasetron (Table 3) [18, 24, 37]. No difference in efficacy was seen in the cisplatin-based study [24], although a significant advantage for ondansetron was observed in one of the two non-cisplatin-based studies (p = 0.01; Fig. 4c). The meta-analytic technique cannot add much to this limited and heterogeneous body of evidence.
Granisetron vs dolasetron
Only three published studies were identified for such a comparison [3, 9, 66] and only one of these met the study inclusion criteria [3]. Therefore, a meta-analysis of these two agents was not possible.
Ondansetron and dolasetron vs palonosetron
Currently, there have only been two studies published that compare ondansetron with palonosetron, one in the moderately emetogenic and one in the highly emetogenic setting, and one study for the comparison of dolasetron with palonosetron (Table 4) [1, 17, 21]. However, there is inadequate data available for a meta-analysis.
Discussion
Current antiemetic guidelines recommend the use of 5-HT3-receptor antagonists as part of combination therapy for management of moderately to highly emetogenic chemotherapy regimens, but do not differentiate between agents, suggesting that they have similar efficacies at equivalent doses [47]. With a high degree of variability seen between small antiemetic studies and conflicting results observed with larger studies (e.g. Gralla et al. [22] and IGARR [27]), a comprehensive combined analysis is warranted. This meta-analysis was therefore designed to evaluate the comparative efficacy of four commonly used 5-HT3-receptor antagonists in the treatment of acute CINV.
Overall analysis of all studies (cisplatin-based and non-cisplatin-based) demonstrated that for acute CINV:
-
1.
granisetron and ondansetron have comparable efficacies at equally potent doses in cisplatin- and non-cisplatin-based studies
-
2.
3 mg granisetron may have superior antiemetic efficacy compared with ondansetron dosed at 8 mg (in moderately emetogenic regimens) and is comparable to ondansetron, 24 or 32 mg
-
3.
no difference in efficacy was found between different doses of granisetron
-
4.
high-dose ondansetron may be more effective than low-dose ondansetron for cisplatin-based chemotherapy, although the results of this analysis are affected by the high degree of variation between the individual trials
-
5.
granisetron is superior to tropisetron in both cisplatin and non-cisplatin-based studies but reached statistical significance only when the results of all studies were combined
-
6.
ondansetron may have similar efficacy to tropisetron (as found in the pooled analysis) but may be superior to dolasetron, although this is based on analysis of just three studies.
Our findings are supported by those of previous analyses, which have suggested comparable efficacy between ondansetron and granisetron [5, 13, 16, 45] and between tropisetron and ondansetron [5].
It has been suggested that ondansetron, at a dose of 8 mg, is suboptimal in controlling acute emesis after non-cisplatin-based chemotherapy (e.g. cyclophosphamide) [12, 14, 16]. The results from the meta-analysis support this, demonstrating that in non-cisplatin-based studies, ondansetron, 8 mg i.v., appears to be inferior to granisetron, 3 mg i.v., although this observation comes from an analysis of small studies that were underpowered. No comparisons were made with the commonly used dose of 1 mg i.v. granisetron due to a lack of studies comparing this dose with ondansetron. The difference observed between high-dose granisetron and low-dose ondansetron may be due to the delayed onset of acute emesis induced by moderately emetogenic chemotherapy regimens combined with the differences in the pharmacological profiles of the two drugs. Granisetron’s longer duration of action within the first 24 h is likely due to its higher affinity to the 5-HT3 receptor and its longer half-life [34, 35, 51]. Strong receptor binding and a longer half-life might be of clinical importance as suggested by studies with palonosetron. Multiple daily doses or a single high dose of ondansetron may therefore be necessary to maintain antiemetic efficacy for 24 h for some patients [8, 47, 72, 73]. In addition, dosing-study analyses demonstrated high-dose ondansetron (24 or 32 mg) are significantly more effective than the low dose (8 mg) for acute antiemetic control. However, the reliability of this finding in the meta-analysis should be treated with caution, as it is affected by significant heterogeneity in the results of the individual trials. Indeed, due to the issue of heterogeneity in some parts of the meta-analysis, it may have been useful to assess individual patient charts, and/or perform further subgroup analyses. However, this was not technically feasible. A high degree of heterogeneity, particularly in the moderately emetogenic setting, reflects increased variation between studies, especially in terms of chemotherapy regimens and individual patient risk factors. For example, factors such as low alcohol intake, previous history of motion sickness, being female [15] and impairment of social activities [30, 54] may lead to a patient being at high risk of developing emesis despite receiving moderately emetogenic therapy. This individual variation is less apparent with cisplatin, as the emetogenicity of this agent tends to mask other variables. Differences between trials also include the trial methodology (e.g. open or blinded), how the endpoints were defined and whether cycles or patients were the unit of observation. It has been suggested that industry sponsorship may have an impact on trial outcome. Whereas a meta-analysis may be a useful tool to assess such influences or bias, this particular analysis is inappropriate due to the weak-to-moderate effects detected.
Dosing schedules are an important variable in terms of cost-effectiveness and it has been suggested that an efficient antiemetic therapy requiring a simple dosing regimen would result in reduced burden on healthcare resources, including time and materials, and may result in an overall reduction in cost. The results of this analysis reinforce the importance of choosing the most appropriate dose of setron, particularly bearing in mind the chemotherapy regimen, to maximize efficacy.
The combined analysis of granisetron vs tropisetron showed a significant advantage for granisetron (p = 0.018) in controlling acute CINV. Interestingly, pharmacogenetic differences have been observed that conceivably affect the metabolism of these agents. Granisetron is the only setron that is not metabolized by the cytochrome P450 (CYP) enzyme, 2D6. This enzyme is subject to genetic polymorphism, resulting in different rates of drug elimination. This was demonstrated in a study by Kaiser et al. [31] who showed that in patients treated with ondansetron or tropisetron, ultra-rapid metabolizers had a significantly higher frequency of vomiting (p < 0.001 within 4 h; p < 0.03 between 5 and 24 h) in the acute phase than all other patients. The difference was more notable in tropisetron-treated patients.
The findings from this meta-analysis do not entirely reflect antiemetic guidelines. In general, the analysis reveals comparable acute antiemetic efficacy between the four 5-HT3-receptor antagonists, with a few exceptions. A significant advantage for granisetron over tropisetron was revealed in a pooled analysis of all chemotherapy regimens studied. The commonly used low-dose ondansetron (8 mg) appears to be not as effective as high-dose ondansetron (24/32 mg) in cisplatin-based studies, or granisetron (3 mg) in non-cisplatin-based studies. However, no studies have been conducted so far comparing a granisetron dose of 1 mg i.v. (or 2 mg orally), which is most commonly used in clinical practice, with low-dose ondansetron. From these results, there seems to be a dose-response relationship for ondansetron, but not for granisetron. Our findings have obvious implications for clinical practice. Whereas the 5-HT3-receptor antagonists included in our analysis appear to have the same antiemetic potential (with the exception of tropisetron), equivalent efficacy is realized only when using equally effective doses. This is of particular importance for any pharmacoeconomic evaluation of antiemetics. To conclude, the emetogenicity of the chemotherapy, the antiemetic drug choice and the dosing regimen of the antiemetic used are all important considerations for administration of the most appropriate and cost-effective 5-HT3-receptor antagonist for the management of acute CINV.
References
Aapro M, Grunberg S, Manikhas G et al (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol 17:1441–1449
Aksoylar S, Akman S, Ozgenc F et al (2001) Comparison of tropisetron and granisetron in the control of nausea and vomiting in children receiving combined cancer chemotherapy. Pediatr Hematol Oncol 18:397–406
Audhuy B, Cappelaere P, Martin M et al (1996) A double-blind, randomised comparison of the anti-emetic efficacy of two intravenous doses of dolasetron mesilate and granisetron in patients receiving high dose cisplatin chemotherapy. Eur J Cancer 32A:807–813
Barrajon E, de las Penas R (2000) Randomised double blind crossover study comparing ondansetron, granisetron and tropisetron. A cost–benefit analysis. Support Care Cancer 8:323–333
Barrajon E, Gasent J (2000) A meta analysis of randomized trials evaluating ondansetron (O), granisetron (G) and tropisetron (T). Proc ASCO 2000 Annual Meeting; (Abstr 2415)
Beck T, Hesketh P, Madajewicz S et al (1992) Stratified, randomized, double-blind comparison of intravenous ondansetron administered as a multiple-dose regimen versus two single-dose regimens in the prevention of cisplatin-induced nausea and vomiting. J Clin Oncol 10:1969–1975
Bonneterre J, Hecquet B (1995) Granisetron (IV) compared with ondansetron (IV plus oral) in the prevention of nausea and vomiting induced by moderately-emetogenic chemotherapy. A cross-over study. Bull Cancer (Paris) 82:1038–1043
Bosnjak S, Neskovic-Konstantinovic Z, Jovanovic-Micic D et al (1996) Single 8 mg dose of oral ondansetron failed to prevent FAC chemotherapy-induced acute nausea and vomiting. J Chemother 8:315–318
Bubalo J, Seelig F, Karbowicz S et al (2001) Randomized open-label trial of dolasetron for the control of nausea and vomiting associated with high-dose chemotherapy with hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 7:439–445
Chiou T-J, Tzeng W-F, Wang S-S et al (2000) Comparison of the efficacy and safety of oral granisetron plus dexamethasone with intravenous ondansetron plus dexamethasone to control nausea and vomiting induced by moderate/severe emetogenic chemotherapy. Chin Med J 63:729–736
Chua D, Sham J, Kwong D et al (2000) Comparative efficacy of three 5-HT3 antagonists (granisetron, ondansetron, and tropisetron) plus dexamethasone for the prevention of cisplatin-induced acute emesis. Am J Clin Oncol 23:185–191
de Wit R, de Boer A, Linden V et al (2001) Effective cross-over to granisetron after failure to ondansetron, a randomized double blind study in patients failing ondansetron plus dexamethasone during the first 24 hours following highly emetogenic chemotherapy. Br J Cancer 85:1099–1101
del Giglio A, Soares H, Caparroz C et al (2000) Granisetron is equivalent to ondansetron for prophylaxis of chemotherapy-induced nausea and vomiting: results of a meta-analysis of randomised controlled trials. Cancer 89:2301–2308
Dempsey CL, Coop AJ, Shillington A et al (2004) Antiemetic effectiveness of ondansetron and granisetron in patients with breast cancer treated with cyclophosphamide. Am J Health-Syst Pharm 61:781–786
Doherty K (1999) Closing the gap in prophylactic antiemetic therapy: patient factors in calculating the emetogenic potential of chemotherapy. Clin J Oncol Nurs 3:113–119
du Bois A (1998) Management der chemotherapie-induzierten Emesis: was ist standard nach 20 Jahren klinischer Forschung? Med Klin 93:3–17
Eisenberg P, Figueroa-Vadillo J, Zamora R et al (2003) Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist: results of a phase III, single-dose trial versus dolasetron. Cancer 98:2473–2482
Fauser A, Duclos B, Chemaissani A et al (1996) Therapeutic equivalence of single oral doses of dolasetron mesilate and multiple doses of ondansetron for the prevention of emesis after moderately emetogenic chemotherapy. Eur J Cancer 9:1523–1529
Forni C, Ferrari S, Loro L et al (2000) Granisetron, tropisetron, and ondansetron in the prevention of acute emesis induced by a combination of cisplatin–Adriamycin and by high-dose ifosfamide delivered in mulitple-day continuous infusions. Support Care Cancer 8:131–133
Gebbia V, Cannata G, Testa A et al (1994) Ondansetron versus granisetron in the prevention of chemotherapy-induced nausea and vomiting. Cancer 74:1945–1552
Gralla R, Lichinitser M, Van Der Vegt S et al (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol 14:1570–1577
Gralla R, Navari R, Hesketh P et al (1998) Single-dose oral granisetron has equivalent antiemetic efficacy to intravenous ondansetron for highly emetogenic cisplatin-based chemotherapy. J Clin Oncol 16:1568–1573
Herrington J, Kwan P, Young R et al (2000) Randomized, multicenter comparison of oral granisetron and oral ondansetron for emetogenic chemotherapy. Pharmacotherapy 20:1318–1323
Hesketh P, Navari R, Grote T (1996) Double-blind, randomized comparison of the antiemetic efficacy of intravenous dolasetron mesylate and intravenous ondansetron in the prevention of acute cisplatin-induced emesis in patients with cancer. Dolasetron Comparative Chemotherapy-induced Emesis Prevention Group. J Clin Oncol 14:2242–2249
Huc P, Block S, Carlier D et al (1998) Oral granisetron versus oral ondansetron for the prevention of nausea and vomiting induced by moderately emetogenic chemotherapies. Bull Cancer (Paris) 85:562–568
Italian Group for Antiemetic Research in Radiotherapy (1999) Radiation-induced emesis: a prospective observational multicenter Italian trial. Int J Radiat Oncol Biol Phys 44:619–625
Italian Group for Antiemetic Research in Radiotherapy (1995) Ondansetron versus granisetron, both combined with dexamethasone, in the prevention of cisplatin-induced emesis. Ann Oncol 6:805–810
Jantunen I, Kataja V, Johansson R (1992) Ondansetron and tropisetron with dexamethasone in the prophylaxis of acute vomiting induced by non-cisplatin-containing chemotherapy. Acta Oncol 31:573–575
Jantunen I, Muhonen T, Kataja V et al (1993) 5-HT3 Receptor antagonists in the prophylaxis of acute vomiting induced by moderately emetogenic chemotherapy—a randomised study. Eur J Cancer 29A:1669–1672
Jordan K, Grothey A, Kegel T et al (2005) Antiemetic efficacy of an oral suspension of granisetron plus dexamethasone and influence of quality of life on risk for nausea and vomiting. Onkologie 28:88–92
Kaiser R, Sezer O, Papies A et al (2002) Patient-tailored antiemetic treatment with 5-hydroxytryptamine type 3 receptor antagonists according to cytochrome P-450 2D6 genotypes. J Clin Oncol 20:2805–2811
Kamanabrou D (1992) Intravenous granisetron—establishing the optimal dose. Eur J Cancer 28A:S6–S11
Krzakowski M, Graham E, Goedhals L et al (1998) A multicenter, double-blind comparison of i.v. and oral administration of ondansetron plus dexamethasone for acute cisplatin-induced emesis. Anti-Cancer Drugs 9:593–598
Kytril tablets prescribing information. Nutley NJ, USA: Roche Laboratories Inc, 2000
Kytril® injection prescribing information. Nutley NJ, USA: Roche Laboratories Inc, 2000
Laszlo J, (1983) Emesis as limiting toxicity in cancer chemotherapy. In: Laszlo J (ed) Antiemetics and cancer chemotherapy. Williams and Wilkins, Baltimore, pp, 1–5
Lofters W, Pater J, Zee B et al (1997) Phase III double-blind comparison of dolasetron mesylate and ondansetron and an evaluation of the additive role of dexamethasone in the prevention of acute and delayed nausea and vomiting due to moderately emetogenic chemotherapy. J Clin Oncol 15:2966–2973
Mabro M, Kerbrat P (1999) Etude comparative du granisetron per os et de l’ondansetron IV chez des patientes recevant une chimiotherapie pour un cancer du sein. Bull Cancer (Paris) 86:295–301
Mantovani G, Maccio A, Bianchi A et al (1996) Comparison of granisetron, ondansetron, and tropisetron in the prophylaxis of acute nausea and vomiting induced by cisplatin for the treatment of head and neck cancer: a randomized controlled trial. Cancer 77:941–948
Martoni A, Angelelli B, Guarldi M et al (1996) An open randomised cross-over study on granisetron versus ondansetron in the prevention of acute emesis induced by moderate dose cisplatin-containing regimens. Eur J Cancer 32A:82–85
Martoni A, Piana E, Strocchi E et al (1988) Comparative crossover trial of two intravenous doses of granisetron (1 mg vs 3 mg) + dexamethasone in the prevention of acute cis-platinum-induced emesis. Anticancer Res 18:2799–2803
Marty M, Kleisbauer J-P, Fournel P et al (1995) Is navoban (tropisetron) as effective as zofran (ondansetron) in cisplatin-induced emesis? Anti-Cancer Drugs 6:15–21
Massidda B, Ionata M (1996) Prevention of delayed emesis by a single intravenous bolus dose of 5-HT3-receptor-antagonist in moderately emetogenic chemotherapy. J Chemother 8:237–242
Massidda B, Laconi S, Foddi M et al (1994) Prevention of non-cisplatin induced emesis: role of the antagonists of 5-HT3 receptors. Ann Oncol 5:204
Mendarte L, Aguas CM, Martinez BE et al (2000) Meta-analysis of granisetron versus ondansetron: efficacy and safety in the prevention of acute emesis induced by high dose cisplatin containing schedules. Med Clin (Barcelona) 115:456–460
Monde M, Grazie M, De Vita F et al (1994) Tropisetron vs granisetron nell’emesi acuta e ri-tardata indotta da cis-platino: dati preliminary. Tumori 80:150 (Abstr 428)
Multinational Association for Supportive Care in Cancer (2005) Antiemetic guidelines from the Consensus Conference on Antiemetic Therapy. Perugia International Cancer Conference VII. Perugia, Italy; 29–31 March 2004. Support Care Cancer 13:77–79; 80–84; 85–96; 97–103; 104–108; 109–111; 112–116; 117–121; 122–128; 129–131
Nakamura H, Taira O, Kodaira S (1999) A multicenter randomized parallel comparison of granisetron injection (GRA) with ondansetron injection (OND) in the acute emesis induced by emetogenic chemotherapy. Proc ASCO 1999 Annual Meeting, (Abstr 2324)
Navari R, Gandara D, Hesketh P et al (1995) Comparative clinical trial of granisetron and ondansetron in the prophylaxis of cisplatin-induced emesis. J Clin Oncol 13:1242–1248
Navari R, Kaplan H, Gralla R et al (1994) Efficacy and safety of granisetron, a selective 5-hydroxytryptamine-3 receptor antagonist, in the prevention of nausea and vomiting induced by high-dose cisplatin. J Clin Oncol 12:2204–2210
Newberry N, Watkins C, Sprosen T et al (1993) BRL 46470 potently antagonizes neural responses activated by 5-HT3 receptors. Neuropharmacology 32:729–735
Noble A, Bremer K, Goedhals L et al (1994) A double-blind, randomised, crossover comparison of granisetron and ondansetron in 5-day fractionated chemotherapy: assessment of efficacy, safety and patient preference. Eur J Cancer 30A:1083–1088
Öge A, Alkis N, Öge O et al (2000) Comparison of granisetron, ondansetron and tropisetron for control of vomiting and nausea induced by cisplatin. J Chemother 12:105–108
Osoba D, Zee B, Warr D et al (1996) Quality of life studies in chemotherapy-induced emesis. Oncology 53(Suppl 1):92–95
Park O, Rha S, Yoo N et al (1997) A comparative study of intravenous granisetron versus intravenous and oral ondansetron in the prevention of nausea and vomiting associated with moderately emetogenic chemotherapy. Am J Clin Oncol 20:569–572
Pectasides D, Mylonakis A, Varthalitis J et al (1997) Comparison of two different doses of ondansetron plus dexamethasone in the prophylaxis of cisplatin-induced emesis. Oncology 54:1–6
Perez E, Hesketh P, Sandbach J et al (1998) Comparison of single-dose oral granisetron versus intravenous ondansetron in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy: a multicenter, double-blind, randomized parallel study. J Clin Oncol 16:754–760
Perez E, Navari R, Kaplan H et al (1997) Efficacy and safety of different doses of granisetron for the prophylaxis of cisplatin-induced emesis. Support Care Cancer 5:31–37
Pinkerton C, Jacobson S, Leclerc J et al (1993) IV granisetron in children receiving highly emetogenic chemotherapy: a double-blind dose ranging study. Eur J Cancer 29A:S200
Ruff P, Paska W, Goedhals L et al (1994) Ondansetron compared with granisetron in the prophylaxis of cisplatin-induced acute emesis: a multicentre double-blind, randomised, parallel-group study. Oncology 51:113–118
Seynaeve C, Schuller J, Buser K et al (1992) Comparison of the anti-emetic efficacy of different doses of ondansetron, given as either a continuous infusion or a single intravenous dose, in acute cisplatin-induced emesis. A multicentre, double-blind, randomised, parallel group study. Br J Cancer 66:192–197
Smith I (1990) A comparison of two dose levels of granisetron in patients receiving moderately emetogenic cytostatic chemotherapy. Eur J Cancer 26:S19–S23
Soukop M (1990) A comparison of two dose levels of granisetron in patients receiving high-dose cisplatin. Eur J Cancer 26:S15–S19
Spector J, Lester E, Chevlen E et al (1998) A comparison of oral ondansetron and intravenous granisetron for the prevention of nausea and emesis associated with cisplatin-based chemotherapy. Oncologist 3:432–438
Stewart A, McQuade B, Cronje J et al (1995) Ondansetron compared with granisetron in the prophylaxis of cyclophosphamide-induced emesis in out-patients: a multicentre, double-blind, double-dummy, randomised, parallel-group study. Oncology 52:202–210
Tan M, Xu R, Seth R (2004) Granisetron vs dolasetron for acute chemotherapy-induced nausea and vomiting (CINV) in high and moderately high emetogenic chemotherapy: an open-label pilot study. Curr Med Res Opin 20:879–882
Tsavaris N, Kosmas M, Vadiaka M et al (2001) Efficacy of ondansetron treatment for acute emesis with different dosing schedules 8 vs 32 mg. A randomized study. J Exp Clin Cancer Res 20:29–34
Whitehead A (2002) Meta-analysis of controlled clinical trials. Wiley, London
Yalçin S, Tekuzman G, Baltali E et al (1999) Serotonin receptor antagonists in prophylaxis of acute and delayed emesis induced by moderately emetogenic, single-day chemotherapy. Am J Clin Oncol 22:94–96
Yusuf S, Peto R, Lewis J et al (1985) Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 27:335–371
Zhang P, Sun Y, Zhang H (1996) A randomized trial of tropisetron in the prophylaxis of nausea and vomiting induced by chemotherapy. Zhonghua Zhongliu Zazhi 18:154–156
Zofran® (ondansetron hydrochloride) injection [US prescribing information]. Research Triangle Park, NC 27709, USA: GlaxoSmithKline
Zofran® (ondansetron hydrochloride) tablets and oral solution [US prescribing information]. Research Triangle Park, NC 27709, USA: GlaxoSmithKline
Acknowledgment
This work was supported by an unrestricted grant from Hoffmann-La Roche. The authors would like to thank Jackie Bannister for the assistance in preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jordan, K., Hinke, A., Grothey, A. et al. A meta-analysis comparing the efficacy of four 5-HT3-receptor antagonists for acute chemotherapy-induced emesis. Support Care Cancer 15, 1023–1033 (2007). https://doi.org/10.1007/s00520-006-0186-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-006-0186-7