Abstract
Objective
Aflibercept (Zaltrap®) is a novel antiangiogenic agent that binds to vascular endothelial growth factor (VEGF) and inhibits VEGF-dependent tumor growth. We aimed to characterize the population pharmacokinetics (PK) of free and bound aflibercept in patients with solid tumors to examine the influence of covariates on their PK and to evaluate the proposed dosing regimens by simulation.
Methods
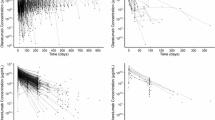
Data from 9 clinical trials with 1,506 cancer patients receiving aflibercept (2–9 mg/kg every 2 or 3 weeks; 1 h IV infusion) as a monotherapy or in combination with various chemotherapies were included. Free and bound aflibercept concentrations were analyzed using a non-linear mixed-effects modeling approach with MONOLIX 4.1.2.
Results
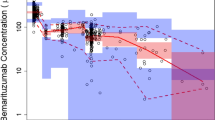
An approximation of a target-mediated drug disposition model with irreversible binding of free aflibercept to VEGF adequately described the PK of free and bound aflibercept. The typical estimated clearances for free (CL f ) and bound aflibercept (CL b ) were 0.88 and 0.19 L/day, respectively. The volumes of distribution for free (V p ) and bound (V b ) aflibercept were similar (~4 L). CL f and V p increased with body weight and were lower in women. Patients with low albumin (ALB) or high alkaline phosphatase (ALK) had faster CL f compared to a typical patient. Pancreatic cancer may be associated with changes in binding of aflibercept to VEGF. Simulations of different dosing regimens showed that adequate saturation of circulating VEGF was achieved with a dose of 4 mg/kg every 2 weeks.
Conclusions
Aflibercept kinetics was most affected by gender, body weight, ALB, ALK and pancreatic cancer. Simulations supported the rationale for the recommended dose of 4 mg/kg every 2 weeks for aflibercept.






Similar content being viewed by others
References
Folkman J (1997) Addressing tumor blood vessels. Nat Biotechnol 15(6):510
Takahashi Y, Kitadai Y, Bucana CD, Cleary KR, Ellis LM (1995) Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis, and proliferation of human colon cancer. Cancer Res 55(18):3964–3968
Takebayashi Y, Aklyama S, Yamada K, Akiba S, Aikou T (1996) Angiogenesis as an unfavorable prognostic factor in human colorectal carcinoma. Cancer 78(2):226–231
Radinsky R, Ellis LM (1996) Molecular determinants in the biology of liver metastasis. Surg Oncol Clin North Am 5(2):215–229
Ferrara N, Davis-Smyth T (1997) The biology of vascular endothelial growth factor. Endocr Rev 18(1):4–25
Gaya A, Tse V (2012) A preclinical and clinical review of aflibercept for the management of cancer. Cancer Treat Rev 38(5):484–493
Sternberg CN (2008) Systemic chemotherapy and new experimental approaches in the treatment of metastatic prostate cancer. Ann Oncol 19(Suppl 7):vii91–vii95
Chu QS (2009) Aflibercept (AVE0005): an alternative strategy for inhibiting tumour angiogenesis by vascular endothelial growth factors. Exp Opin Biol Ther 9(2):263–271
Lockhart AC, Rothenberg ML, Dupont J, Cooper W, Chevalier P, Sternas L, Buzenet G, Koehler E, Sosman JA, Schwartz LH, Gultekin DH, Koutcher JA, Donnelly EF, Andal R, Dancy I, Spriggs DR, Tew WP (2009) Phase I study of intravenous vascular endothelial growth factor trap, aflibercept, in patients with advanced solid tumors. J Clin Oncol 28(2):207–214
Baffert F, Le T, Sennino B, Thurston G, Kuo CJ, Hu-Lowe D, McDonald DM (2006) Cellular changes in normal blood capillaries undergoing regression after inhibition of VEGF signaling. Am J Physiol 290(2):H547–H559
Holash J, Davis S, Papadopoulos N, Croll SD, Ho L, Russell M, Boland P, Leidich R, Hylton D, Burova E, Ioffe E, Huang T, Radziejewski C, Bailey K, Fandl JP, Daly T, Wiegand SJ, Yancopoulos GD, Rudge JS (2002) VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Nat Acad Sci USA 99(17):11393–11398
Eichten A, Adler A, Cooper B, Griffith J, Wei Y, Yancopoulos G, Lin H, Thurston G (2012) Rapid decrease in tumor perfusion following VEGF blockade predicts long-term tumor growth inhibition in preclinical tumor models. Angiogenesis 16(2):429–441
Freyer G, Isambert N, You B, Zanetta S, Falandry C, Favier L, Trillet-Lenoir V, Assadourian S, Soussan-Lazard K, Ziti-Ljajic S, Fumoleau P (2012) Phase I dose-escalation study of aflibercept in combination with docetaxel and cisplatin in patients with advanced solid tumours. British J Cancer 107(4):598–603
Coleman RL, Duska LR, Ramirez PT, Heymach JV, Kamat AA, Modesitt SC, Schmeler KM, Iyer RB, Garcia ME, Miller DL, Jackson EF, Ng CS, Kundra V, Jaffe R, Sood AK (2011) Phase 1–2 study of docetaxel plus aflibercept in patients with recurrent ovarian, primary peritoneal, or fallopian tube cancer. Lancet Oncol 12(12):1109–1117
Colombo N, Mangili G, Mammoliti S, Kalling M, Tholander B, Sternas L, Buzenet G, Chamberlain D (2012) A phase II study of aflibercept in patients with advanced epithelial ovarian cancer and symptomatic malignant ascites. Gynecol Oncol 125(1):42–47
Ramlau R, Gorbunova V, Ciuleanu TE, Novello S, Ozguroglu M, Goksel T, Baldotto C, Bennouna J, Shepherd FA, Le-Guennec S, Rey A, Miller V, Thatcher N, Scagliotti G (2012) Aflibercept and docetaxel versus docetaxel alone after platinum failure in patients with advanced or metastatic non-small-cell lung cancer: a randomized, controlled phase III trial. J Clin Oncol 30(29):3640–3647
He K, Cui B, Li G, Wang H, Jin K, Teng L (2012) The effect of anti-VEGF drugs (bevacizumab and aflibercept) on the survival of patients with metastatic colorectal cancer (mCRC). OncoTargets Ther 5:59–65
Wang TF, Lockhart AC (2012) Aflibercept in the treatment of metastatic colorectal cancer. Clin Med Insights 6:19–30
Van Cutsem E, Tabernero J, Lakomy R, Prenen H, Prausova J, Macarulla T, Ruff P, van Hazel GA, Moiseyenko V, Ferry D, McKendrick J, Polikoff J, Tellier A, Castan R, Allegra C (2012) Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol 30(28):3499–3506
Thai HT, Veyrat-Follet C, Vivier N, Dubruc C, Sanderink G, Mentre F, Comets E (2011) A mechanism-based model for the population pharmacokinetics of free and bound aflibercept in healthy subjects. British J Clin Pharmacol 72(3):402–414
Lavielle M (2008) MONOLIX (MOdèles NOn LInéaires à effets miXtes). MONOLIX group, Orsay, France
Kuhn E, Lavielle M (2005) Maximum likelihood estimation in nonlinear mixed effects models. Comput Stat Data Anal 49(4):1020–1038
Samson A, Lavielle M, Mentre F (2007) The SAEM algorithm for group comparison tests in longitudinal data analysis based on non-linear mixed-effects model. Stat Med 26(27):4860–4875
Wald A (1943) Tests of statistical hypotheses concerning several parameters when the number of observations is large. Trans Am Math Soc 54(3):426–482
Brendel K, Comets E, Laffont C, Laveille C, Mentre F (2006) Metrics for external model evaluation with an application to the population pharmacokinetics of gliclazide. Pharm Res 23(9):2036–2049
Comets E, Brendel K, Mentre F (2008) Computing normalised prediction distribution errors to evaluate nonlinear mixed-effect models: the npde add-on package for R. Comput Methods Programs Biomed 90(2):154–166
Comets E, Brendel K, Mentré F (2010) Model evaluation in nonlinear mixed effect models, with applications to pharmacokinetics. J Soc Fr Stat 151:106–128
Savic RM, Karlsson MO (2009) Importance of shrinkage in empirical Bayes estimates for diagnostics: problems and solutions. AAPS Journal 11(3):558–569
Mager DE, Jusko WJ (2001) General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn 28(6):507–532
Mager DE (2006) Target-mediated drug disposition and dynamics. Biochem Pharmacol 72(1):1–10
Mager DE, Krzyzanski W (2005) Quasi-equilibrium pharmacokinetic model for drugs exhibiting target-mediated drug disposition. Pharm Res 22(10):1589–1596
Gibiansky L, Gibiansky E, Kakkar T, Ma P (2008) Approximations of the target-mediated drug disposition model and identifiability of model parameters. J Pharmacokinet Pharmacodyn 35(5):573–591
Gibiansky L, Gibiansky E (2010) Target-mediated drug disposition: new derivation of the michaelis-menten model, and why it is often sufficient for description of drugs with TMDD. Population Approach Group in Europe. p 19, Abstr 1728. [www.page-meeting.org/?abstract=1728]
Kut C, Mac Gabhann F, Popel AS (2007) Where is VEGF in the body? A meta-analysis of VEGF distribution in cancer. British J Cancer 97(7):978–985
Stefanini MO, Wu FT, Mac Gabhann F, Popel AS (2008) A compartment model of VEGF distribution in blood, healthy and diseased tissues. BMC Syst Biol 2:77
Lu JF, Bruno R, Eppler S, Novotny W, Lum B, Gaudreault J (2008) Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother Pharmacol 62(5):779–786
Fasanmade AA, Adedokun OJ, Ford J, Hernandez D, Johanns J, Hu C, Davis HM, Zhou H (2009) Population pharmacokinetic analysis of infliximab in patients with ulcerative colitis. Eur J Clin Pharmacol 65(12):1211–1228
Kerbel R, Folkman J (2002) Clinical translation of angiogenesis inhibitors. Nat Rev Cancer 2(10):727–739
Li J, Wientjes MG, Au JL (2010) Pancreatic cancer: pathobiology, treatment options, and drug delivery. AAPS J 12(2):223–232
Kindler HL, Niedzwiecki D, Hollis D, Sutherland S, Schrag D, Hurwitz H, Innocenti F, Mulcahy MF, O’Reilly E, Wozniak TF, Picus J, Bhargava P, Mayer RJ, Schilsky RL, Goldberg RM (2010) Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the cancer and Leukemia Group B (CALGB 80303). J Clin Oncol 28(22):3617–3622
Rudge JS, Holash J, Hylton D, Russell M, Jiang S, Leidich R, Papadopoulos N, Pyles EA, Torri A, Wiegand SJ, Thurston G, Stahl N, Yancopoulos GD (2007) VEGF Trap complex formation measures production rates of VEGF, providing a biomarker for predicting efficacious angiogenic blockade. Proc Nat Acad Sci USA 104(47):18363–18370
Conflict of interest
During this work, Hoai-Thu Thai was a PhD student with a research grant funded by Sanofi and UMR 738 INSERM- University Paris Diderot (Head Professor France Mentré) had a research grant from Sanofi. Christine Veyrat-Follet is employee of Sanofi.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thai, HT., Veyrat-Follet, C., Mentré, F. et al. Population pharmacokinetic analysis of free and bound aflibercept in patients with advanced solid tumors. Cancer Chemother Pharmacol 72, 167–180 (2013). https://doi.org/10.1007/s00280-013-2182-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2182-1