Abstract
The rate of long-term remissions after treatment of peripheral T cell lymphomas (PTCL) with standard CHOP-like protocols is unsatisfactory. A prospective multicenter phase II trial was initiated in untreated patients with PTCL of all International Prognostic Index-risk groups, evaluating alemtuzumab consolidation in patients with complete or good partial remission after CHO(E)P-14 induction. Twenty-nine (70.7 %) of the 41 enrolled patients received alemtuzumab consolidation (133 mg in total). The main grades 3–4 toxicities during alemtuzumab therapy were infections and neutropenia with one potentially treatment-related death. Complete responses were seen in 58.5 %, partial responses in 2.4 % and 29.3 % had progressive disease. After a median observation time of 46 months, 19 patients have died, 16 of them due to lymphoma and/or salvage therapy complications. Event-free and overall survival at 3 years in the whole intent to treat population are 32.3 and 62.5 %, respectively, and 42.4 and 75.1 % in the patients who received alemtuzumab. In conclusion, application of a short course of alemtuzumab after CHO(E)P-14 induction is feasible although complicated by severe infections. A current phase III trial, applying alemtuzumab as part of the initial chemotherapy protocol to avoid early progression, will further clarify its significance for the therapeutic outcome.
Similar content being viewed by others
Introduction
Peripheral T cell lymphomas are rare [1], accounting for 5–10 % of all non-Hodgkin lymphomas in Western countries [2]. The most frequent entities according to the WHO classification are peripheral T cell lymphoma not otherwise specified (PTCL-NOS), angioimmunoblastic T cell lymphoma (AITL), extranodal NK/T cell lymphoma and anaplastic large cell T cell lymphoma (ALCL) with and without expression of anaplastic lymphoma kinase (ALK) [3].
Systemic PTCL follow an aggressive clinical course with significantly less favourable outcome than aggressive B cell lymphomas [4, 5]. The International Prognostic Index (IPI) [6] also predicts outcome in PTCL; however, even in the best category, the overall survival (OS) at 5 years is only 50 % [2], excluding patients with ALK + ALCL with an excellent outcome in the IPI 0/1 categories [7].
Treatment with CHOP-like protocols results in overall response rates of 60–70 % but unsatisfactory long-term remissions [7] and a median 5-year OS of only 32 % [3]. Dose-dense CHOP-14 therapy with inclusion of etoposide was recently shown in a retrospective analysis to improve outcome in patients <60 years with normal LDH [8], yielding a 3-year event-free survival (EFS) of 71 versus 51 % for conventional CHOP in ALK + ALCL patients. Although currently recommended as consolidation for high-risk patients in first remission, contradictory results are reported for up-front dose escalation followed by autologous stem cell transplantation (ASCT). Several trials show OS rates comparable to those with conventional regimens, in particular, when ALK + ALCL are excluded [9–11]. Other authors report OS rates of 49 % at 5 years and of 59 % at 4 years [12, 13]. In three prospective trials on up-front ASCT in PTCL, 3-year OS rates of 73 [14], 48 [15] and 56 % [16] were observed.
The monoclonal antibody alemtuzumab targeting the CD52 molecule on B and T cells [17] is an attractive candidate for treatment optimization. Although CD52 expression on malignant T cells varies considerably [18], this antibody showed promising activity in trials of various T cell lymphomas [19–22]. However, its use is complicated by severe opportunistic infections. Reduction of dose and treatment duration has been shown to decrease these complications without compromising the antitumor effect [23].
The rationale of the prospective multicenter phase II DSHNHL 2003–1 study was therefore to combine CHO(E)P-14, an effective chemotherapy for PTCL, with alemtuzumab. The antibody was given to patients in complete response/unconfirmed complete response (CR/CRu) or partial response (PR) after chemotherapy as a short consolidation course to avoid excessive toxicity.
Patients and methods
Patients
The study (NCT Nr. 01806337) was conducted according to the Declaration of Helsinki and approved by the ethics committees of the participating institutions. Patients were enrolled between July 2003 and July 2006 after written informed consent. Inclusion criteria were age 18–70 years, Eastern Cooperative Oncology Group (ECOG) 0–3, previously untreated aggressive PTCL (all IPI), histology of PTCL-NOS (including the lymphoepitheloid Lennert’s variant), AITL, ALK-ALCL and enteropathy-associated intestinal T cell lymphomas (EATL). ALK + ALCL and extranodal T/NK cell lymphomas were excluded as well as patients with major organ dysfunctions other than lymphoma-related, bone marrow infiltration >25 % (quantified by flow cytometry in case of morphological positivity), a history of tuberculosis and overt cytomegalovirus (CMV)-infection, active hepatitis, HIV-positivity, other uncontrolled infections, additional neoplasms and previous radio-chemotherapy. Histological diagnosis was reviewed by a panel of expert haematopathologists.
Treatment schedule
Staging included physical examination, routine laboratory testing, computed tomography scan of neck, chest and abdomen and bone marrow biopsy. Bulky disease was defined as the presence of a tumour mass ≥7.5 cm. A planned complete restaging repeating all of the primary investigations (bone marrow biopsy only in case of involvement) was performed after six chemotherapy cycles (restaging 1). The International Workshop criteria were used for response assessment [24]. After prephase treatment (prednisolone/vincristine), patients <60 years received 6 cycles of CHOEP-14, patients >60 years 6 × CHOP-14 [25], supported by pegfilgrastim 6 mg. Patients with no change (NC) or progression (PRO) went off study. Patients with CR/CRu or PR after chemotherapy received alemtuzumab consolidation (133 mg over 4 weeks) starting 3–6 weeks after the end of chemotherapy. The first three doses were administered intravenously on days 1–3 with dose escalation (3, 10, 30 mg; premedication with clemastin, paracetamol, prednisolone), the following three doses (30 mg) subcutaneously once per week. Prophylaxis against Pneumocystis jirovecii and herpes infections was mandatory and was continued until CD4-cells >200/μl. Patients with positive CMV serology were monitored weekly (pp65, CMV-PCR). Four weeks after completion of the consolidation, a restaging was performed as described above (restaging 2). Patients not receiving alemtuzumab due to reasons other than insufficient chemotherapy response also underwent restaging 2. During the follow-up visits (years 1–2: every 3 months, years 3–5: every 6 months), patients were monitored by physical examination, routine laboratory testing and CT scans (every 6 months).
Statistical analysis
Primary endpoint was the feasibility of alemtuzumab consolidation after a full course of CHO(E)P with assessment of relative dose and toxicity. Secondary endpoints were rate of remission, primary progression, number of patients receiving alemtuzumab, therapy-related mortality, EFS and OS, calculated as the time from registration to the first reported event (PRO, initiation of salvage therapy, additional (unplanned) treatments, relapse or death of any cause) or censored at the most recent assessment date. The analysis was planned as intention-to-treat (ITT) with an additional per protocol analysis (PP) of patients with fulfilled inclusion criteria. The trial was designed to include at least 24 patients with reference diagnosis PTCL-NOS/AITL, receiving alemtuzumab after a full course of chemotherapy. Forty-one patients were registered to allow reliable estimations of the primary endpoint for patients receiving alemtuzumab and to estimate e.g., the complete remission rate for patients with alemtuzumab with a precision of ±18 %. Survival curves were compared with log-rank tests. Relative doses were estimated according to Kaplan–Meier [25]. The significance level was p = 0.050. Statistical analyses were done with SPSS PASW 18.
Results
Patients’ characteristics
Forty-one patients were recruited from 20 institutions and included in the ITT analysis (Table 1). A PP analysis was performed on 37 patients excluding those with incorrect reference histologies: three ALK + ALCL and one extranodal NK cell lymphoma. A considerable number presented with unfavourable prognostic features. Stage III/IV and elevated LDH were more often found in the older cohort. The latter was also more frequent in patients who later did not qualify for alemtuzumab consolidation, whereas other risk factors, such as bulky disease and bone marrow involvement, were present at a higher rate in the alemtuzumab group.
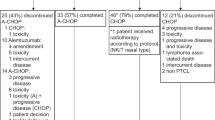
Treatment feasibility
The median duration of the first 5 cycles of CHO(E)P-14 was only slightly longer than planned (77 versus 70 days) with median relative doses of 99.4, 99.8 and 100 % for cyclophosphamide, doxorubicin and etoposide. Dose reduction of vincristine was more frequent in the cohort >60 years, where 24.5 % received less than the complete dose of 6 × 2 mg (6.8 % for <60 years). In the majority of the patients (70.8 %), growth factor support was performed with 6 mg pegfilgrastim according to the study protocol, in some cases substituted by equivalent doses of other G-CSF preparations (23 %, type of G-SCF unknown in 6.2 %) without any difference between the age groups. Thirty-five patients (85.4 %) received all of the planned six chemotherapy cycles (81.5 % < 60 versus 92.9 % >60 years). In six patients, chemotherapy was stopped earlier, predominantly due to early progression (see below and Fig. 1). Therapy with alemtuzumab was started between days 22 and 59 after the end of chemotherapy (median, 34 days) with a median duration of 23 days. Most of the 29 patients qualifying for alemtuzumab (see below) received the planned total dose of 133 mg at the projected time points. Reasons for dose reduction were CMV reactivation (1), severe skin reaction (1) and progression (1). A higher dose was given accidentally to one patient (226 mg).
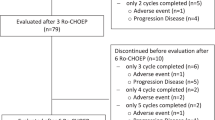
Treatment schedule and clinical course (PRO progressive disease, NC no change, for explanation of “other” see “Treatment response”)
Treatment response
The rate of CR/CRu or good PR after chemotherapy (restaging 1) was 80.5 % (33/41 patients). Eight patients (19.5 %) did not respond sufficiently, four of them showing PRO or NC either early during chemotherapy or shortly afterwards (Fig. 1). They continued treatment off study with various salvage protocols, from conventional salvage regimens to allogeneic stem cell transplantation.
Altogether, 12 patients (29.3 %) did not qualify for alemtuzumab (Fig. 1). Apart from the eight with insufficient response, the reasons were patient’s refusal (1), severe skin exanthema after chemotherapy (1) and reference histology of ALK + ALCL (1). One patient with stage IA disease chemotherapy achieved a CR after three cycles of CHOEP and was treated with involved field irradiation.
The remaining 29 patients (70.7 %) received alemtuzumab consolidation. Among them were two with the retrospective diagnosis of ALK + ALCL and one extranodal NK/T, nasal type, which was unknown at the time of response evaluation after chemotherapy. There was a 60.9 % remission rate at restaging 2 after completion of the whole therapy (ITT, Table 2) with 24 patients still in CR/CRu and one patient remaining in the same status of good PR as after induction chemotherapy. Four patients with CR/Cru or PR at restaging 1 had meanwhile relapsed, two of them under or immediately after alemtuzumab, two of them without (refusal, skin reaction, see above). Considering the whole observation time, relapses (ITT) tended to be more frequent in patients >60 years and there was a non-significant trend to better EFS and OS at 3 years for patients ≤60 years (Fig. 2a, b). In the PP analysis, the EFS at 3 years was 31.4 % [16.3; 46.5 % (95 % confidence interval)] and the OS was 63.9 % [48.2; 79.6 %], thus not essentially different from the complete ITT population (Fig. 2c, d). There was no parameter segregating patients with a good response to chemotherapy and consecutive alemtuzumab consolidation from those with the opposite outcome. Neither sex, age, histology nor the established prognostic markers, such as LDH, IPI, extranodal involvement, were essentially different. For these selected patients who actually received alemtuzumab, the rates for EFS (42.4 % [95 % CI, 23.8–61.0 %]) and OS (75.1 % [95 % CI, 59.0–91.2 %]) were clearly higher than in the whole cohort.
After a median observation time of 46 months, 19 (46.3 %) patients have died. Death was mostly due to lymphoma (13) and/or salvage therapy complications (3). In two patients, lymphoma was complicated by cardiovascular disease and chronic pseudomembranous colitis following CHOEP chemotherapy requiring surgical intervention. There were three additional deaths, the reason for one of them being unknown; however, most probably lymphoma-related since the patient was reported to have relapsed. The two other patients are discussed below.
Treatment toxicity
Adverse events during the initial chemotherapy were comparable to those observed in earlier studies with CHO(E)P-14. Haematotoxicity was the predominant complication with slightly higher rates in the younger group due to addition of etoposide.
The application of alemtuzumab was generally well tolerated. One patient suffered from a severe skin reaction leading to dose reduction, the other patients did not experience any acute grade 3–4 toxicities. Leukocytopenia was the main haematological toxicity. Leukocyte counts <2,000/μl were observed in three patients, two requiring G-CSF support. There was no severe thrombocytopenia or anaemia. Four patients suffered from grades 3–4 infections between 1 and 6 weeks after the last alemtuzumab application: three pneumonias due to Aspergillus spp. and Candida albicans (1) and CMV (2). The fourth patient presented with Gram-negative sepsis following tooth extraction without antibiotic prophylaxis. There were also several less severe infections: Herpes zoster infection 3 weeks after alemtuzumab (1), asymptomatic CMV reactivation during alemtuzumab (3) and fever of unknown origin (1). All patients recovered with appropriate therapy. Eight months after the end of alemtuzumab, there was one fatal course of infection which was potentially treatment-related. This 70-year-old patient, initially with stage IV PTCL-NOS and splenic involvement, experienced prolonged leukopenia following alemtuzumab. Two months after the last restaging, reported as CR, he died from fungal pneumonia with CMV reactivation complicated by cardiac and hepatic failure. One patient developed acute myeloid leukemia (AML) 20 months after completion of therapy with CHOEP and alemtuzumab while still in CR. He died from this disease 13 months later. EBV-related lymphomas were not reported.
Discussion
We could demonstrate that alemtuzumab consolidation after a complete chemotherapy for PTCL was feasible, and nearly all patients received the planned dose of 133 mg within the projected time frame. Grades 3–4 infections were seen in four patients; however, all of them were manageable and with complete recovery. Of note, CMV-pneumonias occurred in spite of close clinical follow-up and CMV monitoring. One of these patients showed grade 3 leukopenia requiring prolonged support with G-CSF and relapsed after several months. The second, still in CR after 46 months, had excessively low CD4-counts remaining <200/μl for almost 1 year. While there is no obvious correlation between relapse and infections in these two cases, the third case of a mixed fungal pneumonia suggests that profound immunosuppression due to disease progression may have contributed to this severe complication. Although in CR at restaging 1 after chemotherapy, the patient who initially had a widely disseminated EATL experienced a fulminant relapse only 2 weeks after recovery from the pneumonia and died shortly afterwards.
No treatment-related death occurred during alemtuzumab application and until 8 months later. There was one fatal course of a 70-year-old patient who died from pneumonia 8 months after the end of therapy. Although persistently low leukocyte counts have certainly contributed to the severe infection, immunosuppression by an incipient lymphoma relapse cannot be excluded. The patient showed high-risk criteria for relapse, the last staging was 2 months ago and a postmortem work-up was not done. Thus, it is difficult to decide whether this death represents a late complication of therapy or is due to the underlying illness.
As another potential late treatment effect, we observed one case of AML in a younger patient receiving CHOEP-14 and alemtuzumab. Since etoposide is known to increase the incidence of secondary AML, this was probably a consequence of chemotherapy rather than of alemtuzumab.
Other trials chose a strategy of concomitant chemotherapy and alemtuzumab. Combination of either CHOP-28 or −21 with alemtuzumab (30 mg/cycle) led to frequent severe infections with two treatment-related deaths [26, 27]. The added effect of alemtuzumab with a total dose almost twice as high as in our study may explain the distinctly higher rate of serious infections. Combination of alemtuzumab (70 mg/cycle) with a fludarabine-containing regimen induced even higher infectious toxicities and six treatment-related deaths [28]. Notably, two cases of EBV-associated lymphoproliferative disease (LPD) were observed several months after therapy. The same phenomenon was encountered in the HOVON study [29], combining CHOP-14 with a very high dose of alemtuzumab (90 mg/cycle). Despite the rather long observation period, there was no such event in our study. This suggests that the total dose of alemtuzumab and/or the timing of alemtuzumab application is critical in this regard.
The potential influence of alemtuzumab on the treatment outcome is difficult to assess. The higher EFS and OS rates (42.4 and 75.1 %) in our alemtuzumab cohort may only reflect the selection effect after omission of those patients who did not respond sufficiently to the initial chemotherapy. Interestingly, a recent study of the GOELAMS group observed similar rates with 41 % EFS at 2 years after CHOP-21 alone [30].
Nevertheless, the high overall remission rates achieved by high alemtuzumab doses concomitant to chemotherapy, ranging between 63 and 90 % [26–29], suggest an added effect. They are higher than in the present study. However, presumably due to the increased rate of side effects, the outcome regarding survival is not essentially different. A 2-year OS and EFS of 53 and 48 % [26] as well as of 55 and 27 % [29] were reported for 30 and 90 mg alemtuzumab per chemotherapy cycle, while OS and EFS in our study were 62.4 and 32.3 % at 3 years.
Surprisingly, this is more or less within the same range as observed with myeloablative protocols [14, 15] although the cytotoxic dose of chemo- and/or radiotherapy in these studies was much higher and the patients clearly younger. Recently, the Nordic Lymphoma Group has reported the final results of the NGT-T-01 trial [16], investigating dose-dense CHO(E)P followed by high-dose chemotherapy and ASCT in treatment-naïve PTCL patients. Although OS rates are confounded by secondary regimens up to allogeneic stem cell transplantation, the 3-year OS (56 %) was not higher than in our study. The 3-year-EFS (32.3 %) used as a secondary endpoint in our study is difficult to compare with TTF and PFS rates since it is based on different criteria. However, the 3-year TTF of 41 % in the NGT-T-01 trial seems promising and may be explained by the relatively high amount of included ALK-ALCL (19 versus 2.4 % in our study), anaplastic histology being associated with significantly better outcome.
We conclude that CHO(E)P-14 followed by a short course of alemtuzumab consolidation is a feasible therapeutic option. Infectious complications are partially severe but mostly manageable and require particular attention. Due to the design of the study, the data do not allow the assessment of the alemtuzumab effect on treatment outcome. However, although representing a selected cohort with favourable characteristics, remission and survival rates in those patients receiving the complete immunochemotherapy are encouraging and comparable to those of more intensive regimens. To definitely clarify if and to what extent the different biological anti-tumour approach of alemtuzumab contributes to the therapeutic outcome, the results of randomized studies such as the current intergroup ACT trials are to be awaited.
References
Foss FM, Zinzani PL, Vose JM et al (2011) Peripheral T-cell lymphoma. Blood 117:6756–6767
Weisenburger DD, Savage KJ, Harris NL et al (2011) Peripheral T-cell lymphoma, not otherwise specified: a report of 340 cases from the International Peripheral T-cell Lymphoma Project. Blood 117:3402–3408
Vose J, Armitage J, Weisenburger D (2008) International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol 26:4124–4130
Akagi T, Takahashi N, Yamaguchi K et al (2011) Comparison of long-term clinical outcomes of CHOP chemotherapy between Japanese patients with nodal peripheral T-cell lymphomas and those with diffuse large B-cell lymphoma in the study group of the Tohoku Hematology Forum. J Clin Exp Hematop 51:29–35
Gisselbrecht C, Gaulard P, Lepage E et al (1998) Prognostic significance of T-cell phenotype in aggressive non-Hodgkin’s lymphomas. Groupe d’Etudes des Lymphomes de l’Adulte (GELA). Blood 92:76–82
The International Non-Hodgkin’s Lymphoma Prognostic Factors Project, Shipp MA, Harrington DP et al (1993) A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med 329:987–994
Savage KJ (2011) Update: peripheral T-cell lymphomas. Curr Hematol Malig Rep 6:222–230
Schmitz N, Trumper L, Ziepert M et al (2010) Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group. Blood 116:3418–3425
Corradini P, Tarella C, Zallio F et al (2006) Long-term follow-up of patients with peripheral T-cell lymphomas treated up-front with high-dose chemotherapy followed by autologous stem cell transplantation. Leukemia 20:1533–1538
Gisselbrecht C, Lepage E, Molina T et al (2002) Shortened first-line high-dose chemotherapy for patients with poor-prognosis aggressive lymphoma. J Clin Oncol 20:2472–2479
Nickelsen M, Ziepert M, Zeynalova S et al (2009) High-dose CHOP plus etoposide (MegaCHOEP) in T-cell lymphoma: a comparative analysis of patients treated within trials of the German High-Grade Non-Hodgkin Lymphoma Study Group (DSHNHL). Ann Oncol 20:1977–1984
Mounier N, Gisselbrecht C, Briere J et al (2004) All aggressive lymphoma subtypes do not share similar outcome after front-line autotransplantation: a matched-control analysis by the Groupe d’Etude des Lymphomes de l’Adulte (GELA). Ann Oncol 15:1790–1797
Kyriakou C, Canals C, Goldstone A et al (2008) High-dose therapy and autologous stem-cell transplantation in angioimmunoblastic lymphoma: complete remission at transplantation is the major determinant of Outcome-Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 26:218–224
Rodriguez J, Conde E, Gutierrez A et al (2007) Frontline autologous stem cell transplantation in high-risk peripheral T-cell lymphoma: a prospective study from The Gel-Tamo Study Group. Eur J Haematol 79:32–38
Reimer P, Rudiger T, Geissinger E et al (2009) Autologous stem-cell transplantation as first-line therapy in peripheral T-cell lymphomas: results of a prospective multicenter study. J Clin Oncol 27:106–113
D’Amore F, Relander T, Lauritzsen GF et al (2012) Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01. J Clin Oncol 30:3093–9
Ginaldi L, De MM, Matutes E et al (1998) Levels of expression of CD52 in normal and leukemic B and T cells: correlation with in vivo therapeutic responses to Campath-1H. Leuk Res 22:185–191
Piccaluga PP, Agostinelli C, Righi S, Zinzani PL, Pileri SA (2007) Expression of CD52 in peripheral T-cell lymphoma. Haematologica 92:566–567
Dearden CE (2006) T-cell prolymphocytic leukemia. Med Oncol 23:17–22
Lundin J, Hagberg H, Repp R et al (2003) Phase 2 study of alemtuzumab (anti-CD52 monoclonal antibody) in patients with advanced mycosis fungoides/Sezary syndrome. Blood 101:4267–4272
Enblad G, Hagberg H, Erlanson M et al (2004) A pilot study of alemtuzumab (anti-CD52 monoclonal antibody) therapy for patients with relapsed or chemotherapy-refractory peripheral T-cell lymphomas. Blood 103:2920–2924
Kim SJ, Kim K, Park Y et al (2012) Dose modification of alemtuzumab in combination with dexamethasone, cytarabine, and cisplatin in patients with relapsed or refractory peripheral T-cell lymphoma: analysis of efficacy and toxicity. Invest New Drugs 30:368–375
Zinzani PL, Alinari L, Tani M et al (2005) Preliminary observations of a phase II study of reduced-dose alemtuzumab treatment in patients with pretreated T-cell lymphoma. Haematologica 90:702–703
Cheson B, Horning SJ, Coiffier B et al (1999) Report of an international workshop to standardize response criteria for non-Hodgkin’s lymphoma. J Clin Oncol 17:1244–1253
Wunderlich A, Kloess M, Reiser M et al (2003) Practicability and acute haematological toxicity of 2- and 3-weekly CHOP and CHOEP chemotherapy for aggressive non-Hodgkin’s lymphoma: results from the NHL-B trial of the German High-Grade Non-Hodgkin’s Lymphoma Study Group (DSHNHL). Ann Oncol 14:881–893
Gallamini A, Zaja F, Patti C et al (2007) Alemtuzumab (Campath-1H) and CHOP chemotherapy as first-line treatment of peripheral T-cell lymphoma: results of a GITIL (Gruppo Italiano Terapie Innovative nei Linfomi) prospective multicenter trial. Blood 110:2316–2323
Kim JG, Sohn SK, Chae YS et al (2007) Alemtuzumab plus CHOP as front-line chemotherapy for patients with peripheral T-cell lymphomas: a phase II study. Cancer Chemother Pharmacol 60:129–134
Weidmann E, Hess G, Chow KU et al (2010) A phase II study of alemtuzumab, fludarabine, cyclophosphamide, and doxorubicin (Campath-FCD) in peripheral T-cell lymphomas. Leuk Lymphoma 51:447–455
Kluin-Nelemans HC, van Marwijk KM, Lugtenburg PJ et al (2011) Intensified alemtuzumab-CHOP therapy for peripheral T-cell lymphoma. Ann Oncol 22:1595–1600
Simon A, Peoch M, Casassus P et al (2010) Upfront VIP-reinforced-ABVD (VIP-rABVD) is not superior to CHOP/21 in newly diagnosed peripheral T cell lymphoma. Results of the randomized phase III trial GOELAMS-LTP95. Brit J Haematol 151:159–166
Acknowledgments
We thank B. Mann and U. Schoenwiese-Thiele for the data management and M. Kunert and B. Wicklein for the database service. The following 20 DSHNHL centers included patients: Zentralklinikum Augsburg (1), Universitätsklinik Bochum (1), Werner Forßmann Klinik Eberswalde (1), Universitätsklinikum Essen (3), Klinikum Fulda (1), Universität Göttingen (10), Katholisches Hospital Hagen (5), Universitätsklinikum Halle/Saale (1), Klinikum St. Georg Hamburg (2), Marienhospital Herne (1), St. Bernward Krankenhaus Hildesheim (1), Universitätsklinken des Saarlandes Homburg (1), Dr. Aldaoud Leipzig (2), Klinikum Großhadern München (2), Schloßbergklinik Oberstaufen (1), Klinikum Oldenburg (1), Ernst-von-Bergmann Klinikum Potsdam (3), Diakoniekrankenhaus Rotenburg (1), Caritas Klinik Saarbrücken (1) and Dr. Horst-Schmidt-Kliniken Wiesbaden (2).
Conflict of interest
Bayer Health Care (Medac Schering Oncology) provided alemtuzumab to all participating centers. Together with AMGEN, Germany, they provided an unrestricted educational grant to the DSHNHL (LT, ML) for the conduct of the trial. There are no other conflicts of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Binder, C., Ziepert, M., Pfreundschuh, M. et al. CHO(E)P-14 followed by alemtuzumab consolidation in untreated peripheral T cell lymphomas: final analysis of a prospective phase II trial. Ann Hematol 92, 1521–1528 (2013). https://doi.org/10.1007/s00277-013-1880-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-013-1880-4